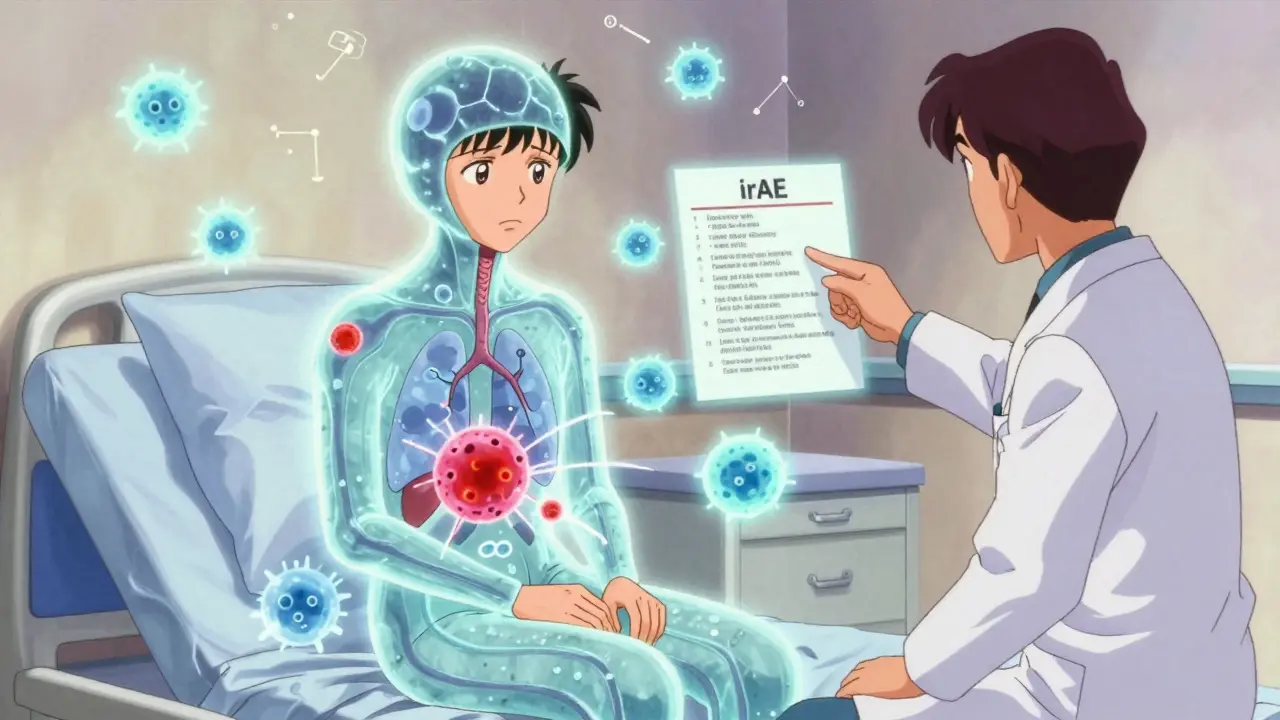
When someone starts treatment with immune checkpoint inhibitors (ICIs) for cancer, the goal is simple: wake up the immune system to fight tumors. But sometimes, the immune system doesn’t stop at cancer. It turns on healthy organs-skin, gut, lungs, even the heart-and causes damage. These unintended side effects are called immune-related adverse events, or irAEs. They’re not rare. In fact, up to 83% of patients on CTLA-4 inhibitors and 72% on PD-1 inhibitors experience at least one. The good news? Most can be managed safely if caught early. The bad news? Many patients and even some doctors miss the early signs.
What Are irAEs and Why Do They Happen?
irAEs happen because immune checkpoint inhibitors block the brakes that normally keep the immune system in check. Drugs like ipilimumab (anti-CTLA-4), pembrolizumab (anti-PD-1), and nivolumab (anti-PD-1) remove those brakes, letting T-cells attack cancer cells. But they can’t tell the difference between a tumor and a healthy tissue. So the immune system starts attacking the thyroid, colon, skin, or liver-thinking it’s fighting cancer.
These reactions look like autoimmune diseases, but they’re not the same. Unlike lupus or rheumatoid arthritis that develop slowly over years, irAEs can show up days or weeks after starting treatment-or even months after stopping. A patient might feel fine for 10 weeks, then suddenly develop diarrhea, rash, or shortness of breath. That’s why monitoring doesn’t stop when treatment ends.
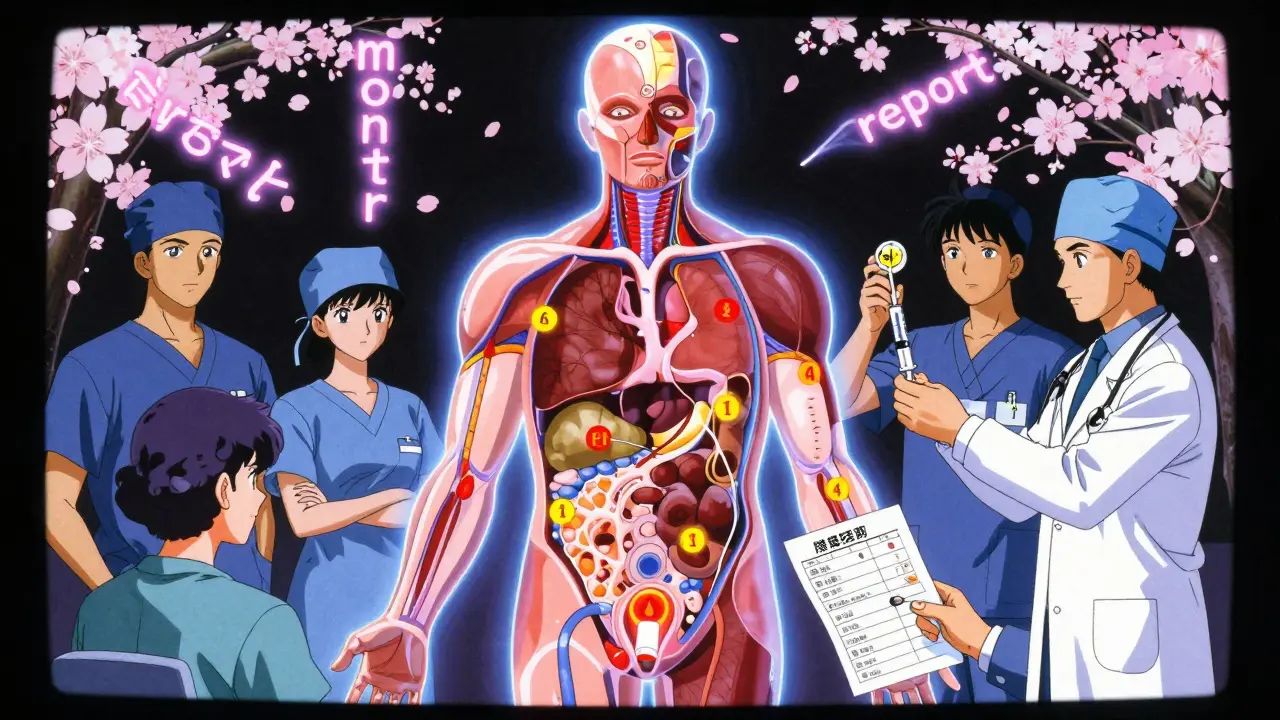
Which Organs Are Most Affected?
Not all irAEs are created equal. Some are common. Others are rare but deadly. Here’s what the data shows:
- Gastrointestinal: Diarrhea and colitis are the most frequent, affecting up to 40% of patients on combination therapy. Severe cases can lead to bowel perforation.
- Endocrine: Thyroid dysfunction (hypo- or hyperthyroidism) happens in 10-20% of patients. Hypophysitis (pituitary inflammation) is rarer but needs hormone replacement, not steroids.
- Dermatologic: Rash, itching, and vitiligo (loss of skin pigment) are common. Vitiligo, oddly enough, is sometimes linked to better cancer response.
- Pulmonary: Pneumonitis (lung inflammation) occurs in 3-5% of patients. It’s one of the deadliest irAEs because symptoms like cough and breathlessness are easy to miss or dismiss.
- Hepatic: Liver enzyme spikes (AST/ALT) show up in 5-10%. If ignored, it can lead to liver failure.
- Neurological: Nerve damage, meningitis, or myasthenia gravis are rare-under 1%-but can be fatal. One study found a 2.7% death rate in patients with cardiac irAEs.
What’s surprising? Endocrine irAEs don’t respond to steroids. If your thyroid shuts down, you don’t need immunosuppression-you need lifelong thyroid hormone pills. Mistaking it for inflammation and giving high-dose prednisone won’t help. It just adds side effects.
How Are irAEs Graded and Treated?
Doctors use the Common Terminology Criteria for Adverse Events (CTCAE) to grade severity. This isn’t just paperwork-it drives treatment.
- Grade 1 (Mild): Skin rash, mild diarrhea. Usually no treatment needed. Just monitor.
- Grade 2 (Moderate): Diarrhea >5 stools/day, moderate rash, elevated liver enzymes. Stop ICI. Start oral prednisolone at 1 mg/kg/day. Symptoms must drop to Grade 1 before restarting treatment.
- Grade 3 (Severe): Diarrhea >10 stools/day, liver enzymes >5x normal, severe rash. Stop ICI. Start IV methylprednisolone (1-2 mg/kg/day) for 3 days, then switch to high-dose oral prednisolone.
- Grade 4 (Life-threatening): Hospitalization needed. ICU-level care. Permanent ICI discontinuation.
Here’s the key: steroids aren’t a one-size-fits-all fix. The taper matters. Rushing it causes rebound symptoms. A typical taper lasts 4-6 weeks. Some patients need to go from 60 mg of prednisone down to 5 mg over two months. That’s a long time to deal with insomnia, weight gain, or mood swings.
What If Steroids Don’t Work?
One in five patients don’t improve after 48 hours of high-dose steroids. That’s called steroid-refractory irAE. When that happens, doctors reach for stronger tools:
- Infliximab: A TNF-alpha blocker. First-line for colitis and some cases of pneumonitis. Given as IV infusion.
- Vedolizumab: Newer option for gut issues. Targets gut-specific immune cells. A 2024 SITC guideline showed 68% response rate in steroid-refractory colitis.
- Mycophenolate mofetil: Used for liver or lung inflammation. Slows immune cell production.
- IVIG: Packed antibodies from donors. Used for neurological or hematologic irAEs.
- Cyclophosphamide: Last-resort for severe, life-threatening cases.
Important: Using these drugs doesn’t kill the cancer treatment. Multiple studies confirm patients still respond to immunotherapy even after being on infliximab or IVIG. The fear that immunosuppression weakens the anti-tumor effect? It’s outdated.
Why Timing and Communication Matter
One of the biggest problems? Delayed reporting. Patients often think, “It’s just a rash,” or “I’m tired because of chemo,” and wait. But early intervention cuts hospitalization rates in half. Real-world data from Flatiron Health shows that if patients get help within 48 hours of symptom onset, hospitalization drops from 34% to 19%.
And yet, 79% of oncology nurses say patients don’t understand what to watch for. A patient on pembrolizumab might get diarrhea and assume it’s food poisoning. They wait three days. By then, their colon is inflamed. A simple stool test and steroid could’ve stopped it.
That’s why education is part of the treatment. Leading centers now give patients printed checklists: “Call your oncologist if you have…” with clear symptoms for each organ. Some clinics use automated alerts in electronic records-when a patient logs “3+ loose stools” in a portal, the system flags it and nudges the care team.
What About Long-Term Effects?
Most irAEs resolve. About 85-90% of patients fully recover. But 10-15% develop chronic issues. Thyroid damage? Lifelong hormone pills. Diabetes from pancreas inflammation? Daily insulin. Lung scarring from pneumonitis? Oxygen therapy. This isn’t a one-time event-it’s a new health condition.
And steroid side effects? They’re brutal. A 2023 survey of 45 patients found:
- 72% had trouble sleeping
- 65% gained 10+ pounds
- 58% felt anxious or depressed
That’s why tapering slowly isn’t just medical-it’s psychological. Rushing it makes patients feel worse. Slowing it down gives their body time to adjust.
How Are Hospitals Getting Better?
Five years ago, community oncology clinics had no plan for irAEs. Now, those with dedicated immune toxicity teams have 92% protocol adherence. Those without? Only 68%. The difference? Structure.
- 24/7 access to endocrinologists, gastroenterologists, and pulmonologists
- Pre-written order sets for steroid dosing
- Automated alerts in EHRs (like Epic’s 2023 update)
- Monthly case reviews with neurology and dermatology
One study showed that after implementing a formal irAE protocol, severe complications dropped by 37% in just 18 months. That’s not just better care-it’s saving lives.
What’s Next?
The future is in prediction. A 2023 study in Nature Medicine found that if a patient’s baseline IL-17 blood level is above 5.2 pg/mL, they’re 4.7 times more likely to develop a severe irAE. That’s not just science-it’s a warning light.
Meanwhile, ESMO is rolling out patient education materials in 15 languages. Because if a patient doesn’t know what a “Grade 2 colitis” looks like, they won’t call for help. And if they don’t call, the damage can be irreversible.
As more patients get combination immunotherapies (over 287 are now in trials), irAEs will become more common-and more complex. The answer isn’t just more drugs. It’s better systems, smarter alerts, and patients who know exactly when to speak up.
Can irAEs happen after stopping immunotherapy?
Yes. While most irAEs show up within the first 3 months of treatment, they can appear weeks or even months after stopping immune checkpoint inhibitors. This is why ongoing monitoring is critical-even after treatment ends. Patients should be advised to report new symptoms like diarrhea, rash, shortness of breath, or fatigue to their oncologist immediately, regardless of when they last received therapy.
Do steroids reduce the effectiveness of cancer treatment?
No. Multiple studies have shown that using corticosteroids or other immunosuppressants to treat irAEs does not reduce the anti-cancer effect of immune checkpoint inhibitors. Early concerns that suppressing the immune system might weaken tumor control have been disproven. Patients treated with infliximab, IVIG, or high-dose steroids still achieve durable responses to immunotherapy.
Are all irAEs treated with steroids?
No. Endocrine irAEs-like thyroid dysfunction, hypophysitis, or adrenal insufficiency-require hormone replacement, not steroids. For example, low thyroid hormone levels need levothyroxine, not prednisone. Giving steroids in these cases won’t fix the problem and may cause unnecessary side effects. Always check hormone levels before assuming it’s inflammation.
What should I do if I develop a rash during immunotherapy?
Don’t ignore it. Even a mild rash can be the first sign of a more serious irAE. Contact your oncology team immediately. They’ll assess whether it’s a simple allergic reaction or an immune-related rash. If it’s Grade 2 or higher, they’ll likely stop immunotherapy and start oral steroids. Avoid over-the-counter creams unless approved-some can worsen inflammation. Document how it looks, where it spreads, and if it itches or burns.
Can irAEs be prevented?
There’s no guaranteed way to prevent irAEs, but early detection is the best strategy. Blood tests before each infusion (like liver enzymes, TSH, and creatinine) help catch problems early. Some centers now check baseline IL-17 levels to identify high-risk patients. Patients should be given clear instructions on symptoms to watch for and how to report them quickly. Staying vigilant and communicating with your care team reduces the chance of severe complications.