When you pick up a generic pill at the pharmacy, you might think it’s just a cheaper version of the brand-name drug. But here’s the truth: every generic drug approved by the FDA has to meet the same strict standards for safety, quality, and strength as the original. There’s no cutting corners. No shortcuts. If it doesn’t match the brand-name drug exactly in how it works inside your body, it doesn’t get approved.
What Makes a Generic Drug Approved?
The FDA doesn’t require generic manufacturers to run new clinical trials on thousands of patients. That’s because they don’t need to prove the drug works - the brand-name version already did that. Instead, generic makers use an abbreviated pathway called an ANDA, or Abbreviated New Drug Application. But don’t let the word “abbreviated” fool you. This process is one of the most technically demanding in all of pharmaceutical regulation.
To get approved, a generic drug must have the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. That means if the original is a 10mg tablet taken by mouth, the generic must be identical in every physical way. Even the inactive ingredients - like fillers or coatings - must be safe and not affect how the drug is absorbed.
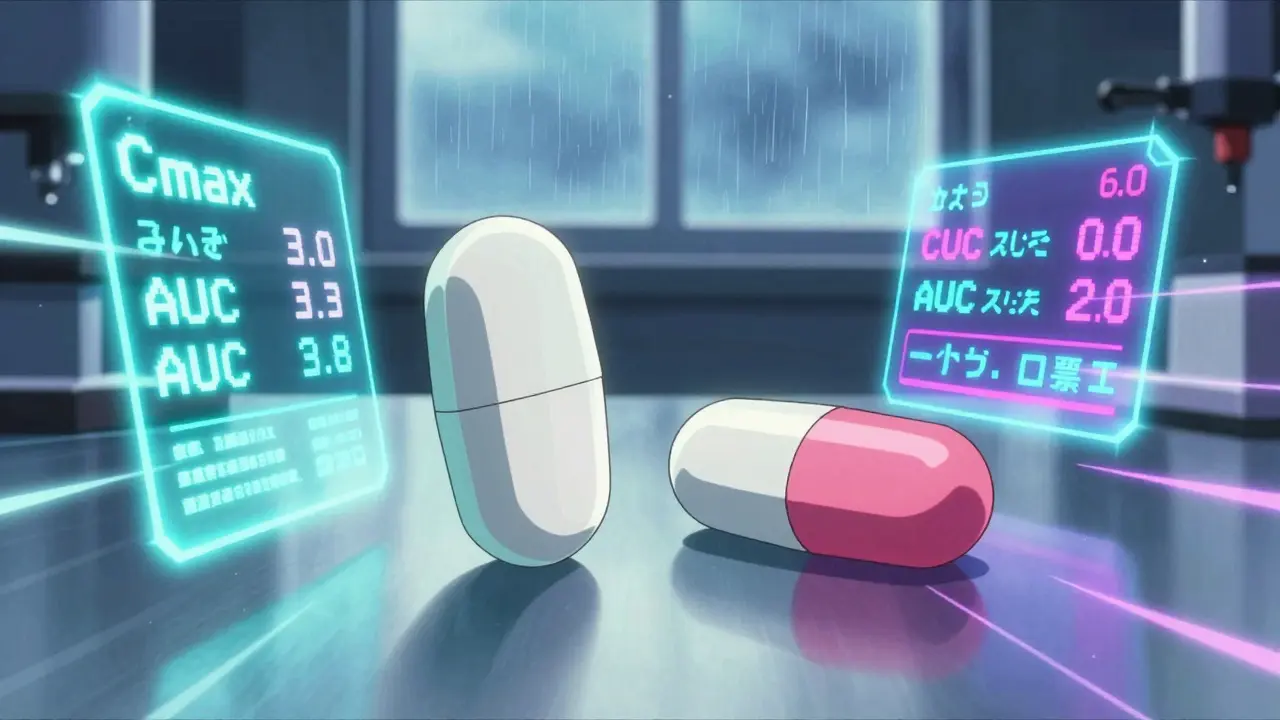
The real test? Bioequivalence. This isn’t just a buzzword. It’s a hard scientific measurement. The FDA requires that the generic drug enters your bloodstream at the same rate and to the same extent as the brand-name version. Specifically, the amount of drug in your blood - measured by Cmax and AUC values - must fall between 80% and 125% of the brand-name drug’s levels. That’s a 45% window, but it’s not arbitrary. It’s based on decades of clinical data showing that within this range, there’s no meaningful difference in how the drug performs in patients.
How Do They Prove It?
Manufacturers run bioequivalence studies in healthy volunteers. Usually, it’s 24 to 36 people who take both the brand-name drug and the generic, in random order, with a washout period in between. Blood samples are taken over 24 to 72 hours to track how quickly and completely the drug is absorbed.
For simple pills like ibuprofen or metformin, this is straightforward. But for complex drugs - like extended-release versions, inhalers, or topical creams - it gets much harder. Take Ritalin LA, for example. It’s designed to release methylphenidate slowly over 12 hours. The generic version can’t just match total absorption; it has to match the release pattern at specific time points: 0-3 hours, 3-7 hours, and 7-12 hours. If the generic releases too fast at first, it could cause side effects. Too slow, and it won’t work all day. The FDA requires partial AUC measurements to make sure it’s right.
For drugs with a narrow therapeutic index - like warfarin, levothyroxine, or cyclosporine - the window is even tighter. The FDA now requires a 90% to 111% range for these. One study found that patients switching between different generic versions of levothyroxine had slight fluctuations in thyroid hormone levels when the bioequivalence range was wider. So the FDA tightened it to 95%-105%. That’s precision engineering for your hormones.
Manufacturing Isn’t Just About the Pill
A generic drug isn’t approved just because the active ingredient matches. The entire manufacturing process must be controlled to the same standard as the brand-name drug. That’s where Current Good Manufacturing Practices (cGMP) come in.
The FDA inspects every facility that makes generic drugs - over 1,200 pre-approval inspections each year. These aren’t surprise visits. Companies submit detailed documentation showing how they make each batch: temperature controls, mixing times, tablet hardness, dissolution rates. They must prove consistency across three consecutive commercial-scale batches. One company, Hetero Labs, got a Complete Response Letter from the FDA in 2021 because their generic version of Jardiance had inconsistent tablet hardness. That’s not a minor issue. If tablets vary in hardness, they dissolve at different rates. That changes absorption. That changes effectiveness.
Even the packaging matters. A generic epinephrine auto-injector isn’t just a cheaper pen. It has to deliver the same dose, at the same speed, with the same reliability as the EpiPen. Between 2015 and 2020, the FDA approved only 3 out of 27 generic EpiPen applications. Why? The device design - the spring mechanism, needle depth, activation force - had to match exactly. That’s not chemistry. That’s mechanical engineering.

Why Do So Many Applications Get Rejected?
Even though the pathway is “abbreviated,” less than 10% of generic applications get approved on the first try. That’s not because the FDA is being difficult. It’s because the bar is set high, and many applicants underestimate how detailed the requirements are.
Common reasons for rejection? Incomplete chemistry data. Poorly designed bioequivalence studies. Inadequate process validation. Missing stability data. One manufacturer submitted a generic version of a blood pressure drug but didn’t test it under high humidity. The tablets crumbled. The FDA rejected it. Another tried to save money by using a different manufacturing solvent. The impurity profile didn’t match. Rejected.
Complex generics - like injectables, inhalers, or topical gels - face even higher rejection rates. A 2021 analysis showed only 58% of complex generic applications were approved within three review cycles, compared to 76% for simple pills. That’s why the FDA has a Pre-ANDA program. Over 78% of successful applicants use it. They meet with FDA scientists months before submitting to iron out problems early. It’s not optional for complex products. It’s essential.
How Long Does It Take? How Much Does It Cost?
Bringing a brand-name drug to market costs $2.6 billion. A generic? Around $1.3 million. But that doesn’t mean it’s easy or cheap to get right.
The average time from submission to approval is 32.7 months. For complex generics, it’s nearly 47 months. Why? Because the FDA reviews every page of the application - often 5,000 to 10,000 pages - with a team of chemists, pharmacologists, and engineers. They check every study, every specification, every batch record.
And it’s not just the FDA. The manufacturing site has to be inspected. The supply chain has to be validated. The labeling has to match exactly. Even the font size on the box matters if it affects patient understanding.
Are Generic Drugs Really the Same?
Yes. And the data proves it.
A 15-year study of post-market outcomes showed that 98.7% of generic drugs performed the same as their brand-name counterparts in real-world use. That’s not just clinical trials. That’s millions of patients over years. The American Medical Association confirmed this in 2021. The FDA’s own data shows that generics account for 90% of prescriptions in the U.S. but only 23% of drug spending. That’s $373 billion saved in 2022 alone.
There are rare cases where patients report differences - usually with narrow therapeutic index drugs. But those are usually due to switching between different generic brands, not because the FDA’s standards are weak. The FDA addresses this by requiring tighter bioequivalence limits and encouraging patients to stick with the same generic manufacturer when possible.
What’s Changing Now?
The FDA is pushing to improve approval times for complex generics. By 2027, they aim to approve 50% of these applications within two review cycles - up from just 28% today. They’re also working with global regulators to harmonize standards, so a generic approved in the U.S. meets the same quality bar as one approved in Europe or Japan.
And new complex drugs are emerging. The first generic of Humira, a $20 billion-a-year biologic, was approved in December 2023. The first generic of Vivitrol, a monthly injectable for opioid addiction, came in August 2023. These aren’t simple pills. They’re sophisticated products requiring advanced science and manufacturing.
But the core hasn’t changed. Whether it’s a $2 generic aspirin or a $2,000 generic cancer drug, the FDA’s job is the same: make sure it’s safe. Make sure it works. Make sure it’s the same as the brand.
What You Should Know
If you’re prescribed a generic drug, you can trust it. The FDA doesn’t approve anything that doesn’t meet the same standards as the original. The only real difference? The price. And the savings.
For patients, that means more access. For the system, it means lower costs. For manufacturers, it means a tough but fair path to market. And for the public? It means confidence that the medicine you take - no matter the label - has been held to the highest possible standard.
Are generic drugs as safe as brand-name drugs?
Yes. Every generic drug approved by the FDA must meet the same strict standards for safety, strength, purity, and quality as the brand-name version. The FDA requires bioequivalence testing to prove the generic delivers the same amount of active ingredient into your bloodstream at the same rate. Post-market surveillance over 15 years shows that 98.7% of generic drugs perform identically to their brand-name counterparts in real-world use.
Why do some people say generics don’t work as well?
Occasionally, patients report differences when switching between different generic versions - especially with narrow therapeutic index drugs like warfarin or levothyroxine. This isn’t because the generics are unsafe, but because switching between different manufacturers can cause slight variations in inactive ingredients or release patterns. The FDA requires tighter bioequivalence limits (95%-105%) for these drugs and recommends patients stick with the same generic brand once they’ve found one that works.
How does the FDA ensure generic drugs are made in clean facilities?
The FDA inspects every manufacturing site before approving a generic drug. Over 1,200 pre-approval inspections are conducted each year. Facilities must comply with Current Good Manufacturing Practices (cGMP), which require strict controls over every step of production - from raw materials to packaging. If a facility has serious deficiencies, the application is delayed until corrections are verified.
What’s the difference between a generic drug and a biosimilar?
Generics are exact copies of small-molecule drugs, like aspirin or metformin. Biosimilars are highly similar versions of complex biological drugs, like Humira or insulin. Because biological drugs are made from living cells, they can’t be exact copies. Biosimilars require more clinical testing than generics to prove they work the same way. The FDA treats them as separate pathways.
Why do some generic drugs take years to reach the market after approval?
Even after FDA approval, a generic drug can be delayed by patent lawsuits or exclusivity rights held by the brand-name company. The FTC found that on average, generic entry is delayed by 2.4 years after approval due to legal tactics like “evergreening” - where companies make minor changes to patents to block competition. Regulatory approval doesn’t guarantee immediate market access.
What Comes Next?
If you’re a patient, stick with your prescribed generic unless you notice a change in how you feel. Talk to your pharmacist or doctor before switching brands.
If you’re a manufacturer, don’t skip the Pre-ANDA meetings. Use them. The FDA offers over 1,200 of them each year - and 85% of companies that use them report higher success rates.
If you’re just curious - remember this: the next time you save money on a prescription, you’re not getting a lesser product. You’re getting a drug that passed the same tests, in the same labs, under the same rules as the brand. That’s not luck. That’s science.
Lisa Davies
December 16, 2025 AT 10:27Melissa Taylor
December 17, 2025 AT 04:28Jake Sinatra
December 17, 2025 AT 12:44John Brown
December 18, 2025 AT 19:43Christina Bischof
December 19, 2025 AT 02:19Jocelyn Lachapelle
December 19, 2025 AT 14:07Mike Nordby
December 21, 2025 AT 02:55Michelle M
December 21, 2025 AT 23:51Nupur Vimal
December 23, 2025 AT 04:21RONALD Randolph
December 24, 2025 AT 19:35Raj Kumar
December 25, 2025 AT 00:49Sai Nguyen
December 25, 2025 AT 15:56Cassie Henriques
December 27, 2025 AT 12:36John Samuel
December 29, 2025 AT 08:48