Why Physical Therapy Works When Medications Don’t
Medications can mask pain, but they don’t fix what’s broken. If you’ve been popping pills for months and still feel stiff, achy, or burned out, you’re not alone. Physical therapy doesn’t just numb the pain-it rebuilds the system causing it. The science is clear: structured movement, targeted stretching, and gradual restoration of function reduce pain more effectively than drugs for most chronic conditions. A 2023 study in the Journal of Orthopaedic & Sports Physical Therapy found that 50-75% of people saw major pain drops in just 6-8 weeks with the right physical therapy plan. No prescriptions. No side effects. Just your body learning to move again.
The Three Pillars: Exercise, Stretching, Restoration
Physical therapy for pain isn’t one thing-it’s three things working together. First, exercise trains your muscles to support your joints and triggers your body’s natural painkillers. Second, stretching releases tight tissues that pull on nerves and joints, often the hidden source of discomfort. Third, restoration means relearning how to move without pain-walking, bending, reaching-so it doesn’t come back.
These aren’t random workouts. They’re precise, research-backed routines. For example, aerobic exercise like walking or swimming at 65-75% of your maximum heart rate for 20 minutes releases endorphins and reduces inflammation. Strength training with 2-3 sets of 8-15 reps at 60-80% of your one-rep max rebuilds muscle that’s been weakened by pain. And stretching? Hold each stretch 30-60 seconds, 5-7 days a week. That’s it. No need to push to the point of agony. Consistency beats intensity every time.
What Kind of Exercise Works Best?
Not all movement is equal when it comes to pain. High-impact activities like running can make knee or back pain worse. Low-impact options do the job better-and safer.
- Walking: The simplest tool. Studies show it reduces osteoarthritis pain by 35-40%. Start with 10 minutes, add 2-3 minutes every few days.
- Swimming or water aerobics: Water cuts joint stress by half. Perfect for arthritis or spine pain. You get resistance without pounding.
- Cycling: Stationary or outdoor, it’s gentle on knees and hips. Adjust resistance so you can talk but not sing.
- Tai chi: For fibromyalgia or widespread pain, tai chi beats regular cardio. One 2022 trial found 30% more pain relief after 12 weeks.
- Resistance bands: Cheap, portable, and powerful. A 2-minute routine with bands can cut neck and shoulder pain by 28%.
High-intensity workouts? Avoid them if you have fibromyalgia or chronic pain. A 2020 review found 22% of people had worse pain after intense sessions. Moderate is the sweet spot.
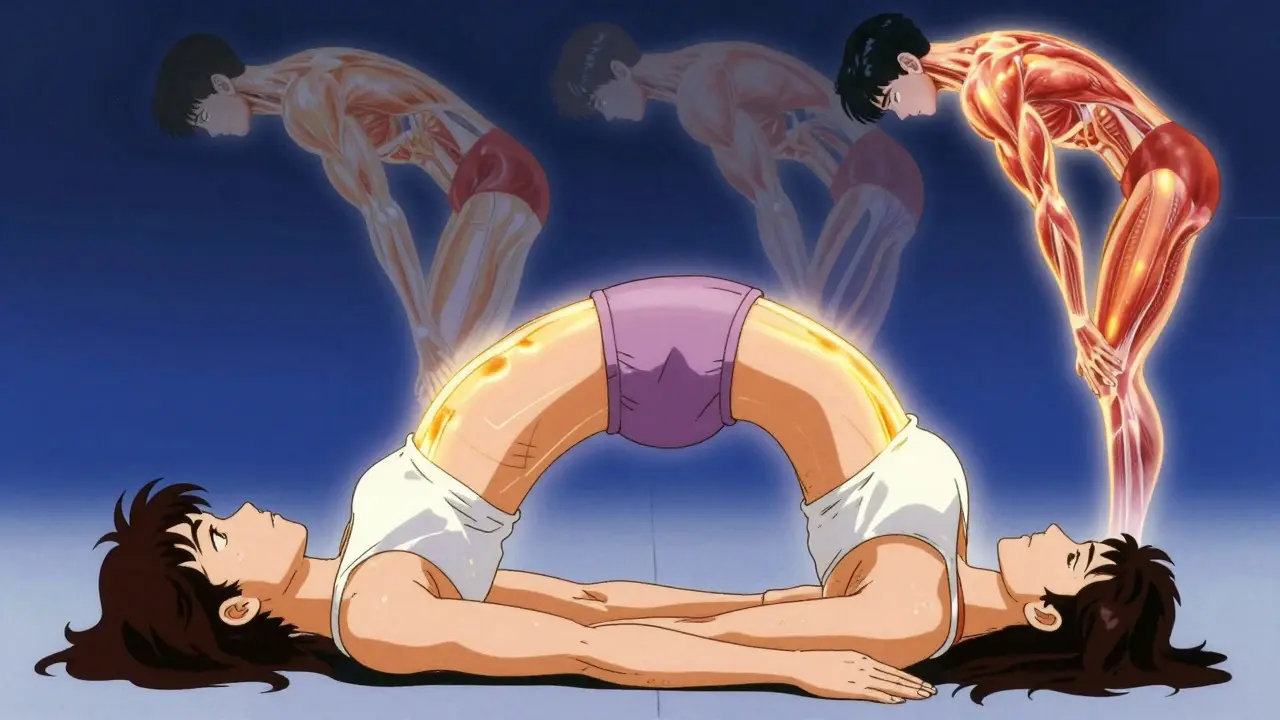
Stretching Isn’t Just Touching Your Toes
Stretching for pain isn’t about flexibility contests. It’s about releasing tension that’s trapped in muscles, tendons, and fascia. Think of it like untangling a knot-not yanking, but gently working it loose.
For lower back pain, try the cat-cow stretch: on hands and knees, arch your back up like a cat, then drop it down like a cow. Do 10 slow reps. For tight hips, the figure-four stretch works wonders. Sit on a chair, cross one ankle over the opposite knee, and gently lean forward until you feel a stretch in the hip. Hold 30 seconds. Switch sides.
Key rule: never bounce. Hold the stretch. Breathe deeply. If it hurts more than a 3 out of 10, you’re pushing too hard. Pain during stretching? That’s a red flag. Discomfort? Normal. Sharp pain? Stop.
Restoration: Relearning Movement Without Fear
Pain changes how you move. You start limping, hunching, avoiding certain motions. Over time, your body forgets how to move properly-and that makes pain worse. Restoration is about undoing that.
Physical therapists use graded activity: small, safe increases in movement. If you can walk 10 minutes without pain spiking above 3/10, next week you walk 11. And so on. The goal isn’t to push through pain. It’s to prove to your nervous system that movement is safe.
One common mistake? People think they need to be pain-free before they move. That’s backwards. You move to get pain-free. The 2-hour rule is your guide: if pain returns to baseline within 2 hours after exercise, you’re on track. If it lingers longer, scale back.
For back pain, strengthening your core and glutes is critical. Dr. James Fricton from UT Health Austin says properly done home exercises reduce chronic back pain by 70%. Simple moves like bridges (lying on your back, lifting hips) and bird-dogs (on hands and knees, extending opposite arm and leg) rebuild support you didn’t know you’d lost.
Real People, Real Results
Reddit’s r/Physical_Therapy community has over 140,000 members sharing stories. One user, u/ChronicPainWarrior, cut fibromyalgia pain by 80% after 16 weeks of daily tai chi. Another, u/BackPainSufferer, dropped sciatica pain from 7/10 to 2/10 in three weeks with straight leg raises.
But not everyone succeeds. A 2023 review of Healthgrades reviews found 42% of negative experiences came from exercises that made pain worse-usually because form was wrong. That’s why starting with a therapist matters. Two or three supervised sessions teach you the right way to move. After that, video demos help you stay on track. One VA study showed adherence jumped from 45% to 78% when patients got video instructions.
The Arthritis Foundation’s two-minute exercise routine-designed for office workers with neck and shoulder pain-got 87% positive feedback. People did it while waiting for coffee or between Zoom calls. That’s the power of micro-movements. You don’t need an hour. You need consistency.
What’s Holding People Back?
Physical therapy works. So why don’t more people do it?
One big reason: therapists aren’t always trained to prescribe it. A 2024 Physiopedia survey found 68% of physical therapists feel underprepared to give clear exercise advice. That means you might get vague instructions like “stay active” instead of a real plan.
Another issue: time and cost. Corporate clinics often squeeze patients into 30-minute slots with 2-3 others. Academic centers offer 45-minute one-on-one sessions-but they’re harder to access. Medicare covers 80% of approved therapy, but you still need a referral.
And then there’s fear. Many people think, “If it hurts, I shouldn’t move.” But pain doesn’t equal damage. It’s often a warning light, not a stop sign. Learning to move within a safe range is the key.
The Future: More Personalized, More Accessible
Physical therapy is changing fast. In January 2024, the Arthritis Foundation expanded its two-minute routine to cover 12 joint conditions. Mayo Clinic released a 15-minute back exercise protocol in March 2024 that helped 62% of patients cut pain by half in six weeks-with 92% sticking with it.
Telehealth is growing. 63% of clinics now offer virtual sessions. Wearable sensors track your movement and give feedback. The NIH just funded $14.7 million to study ultra-short exercise routines for chronic pain. The goal? Make effective therapy fit into your life, not the other way around.
By 2028, physical therapy is projected to grow nearly 18% a year. Why? Because the opioid crisis forced healthcare to find better ways. The American College of Physicians now says physical therapy, exercise, and spinal manipulation should come before pills for back pain.
How to Start Today
You don’t need a fancy gym or a prescription. Start small.
- Choose one low-impact activity: walking, swimming, or cycling. Do it for 10 minutes, three times this week.
- Add two stretches: cat-cow for your back, figure-four for your hips. Hold each 30 seconds. Do them every morning.
- Use the 2-hour rule: if pain returns to normal within 2 hours after moving, keep going. If it lasts longer, reduce intensity.
- Track your pain daily on a scale of 0-10. You’ll see patterns.
- If you’re not improving in 3-4 weeks, find a physical therapist who specializes in pain-not just sports injuries.
Remember: physical therapy isn’t a quick fix. It’s a reset. It’s your body relearning how to carry you without pain. It takes patience. But the payoff? Walking without wincing. Sleeping through the night. Getting up without that first stiff groan. That’s worth every minute.
Can physical therapy help with chronic pain even if I’ve had it for years?
Yes. Chronic pain doesn’t mean your body is broken beyond repair. It means your nervous system has become overly sensitive. Physical therapy retrains that system. Studies show people with 10+ years of pain still get 50-70% relief with consistent, properly guided exercise and stretching. The key is matching the protocol to your condition-not giving up because it’s been a long time.
Do I need a doctor’s referral to see a physical therapist?
In the UK and many US states, you can see a physical therapist directly without a referral-this is called direct access. But insurance, including Medicare, often requires one for coverage. Check with your provider. Even if you don’t need a referral, a doctor’s diagnosis helps your therapist tailor the plan to your specific pain source, like arthritis, herniated disc, or nerve compression.
What if exercise makes my pain worse?
Some discomfort is normal, especially at first. But sharp, shooting, or radiating pain isn’t. Use the 2-hour rule: if pain returns to baseline within two hours after exercise, you’re safe to continue. If it’s still elevated, you pushed too hard. Scale back intensity, reduce duration, or switch to a gentler movement. Never ignore pain that lingers or spreads. That’s a signal to pause and reassess.
Is stretching better than strengthening for pain relief?
Neither works alone. Stretching releases tight tissues that pull on joints. Strengthening builds support so those joints don’t get overloaded. For example, tight hamstrings can pull on your lower back-stretching helps. But weak glutes can’t stabilize your pelvis-strengthening fixes that. The best results come from combining both. Think of it like fixing a wobbly chair: you need to loosen the screws (stretch) and tighten the legs (strengthen).
How long until I feel better with physical therapy?
Most people notice small improvements in 2-3 weeks-better sleep, less stiffness in the morning. Major pain reduction usually takes 6-8 weeks with consistent effort. That’s when muscle strength, joint mobility, and nervous system sensitivity begin to shift. Don’t expect miracles in a week. But if you stick with it, most people report life-changing results by week 10.
Can I do physical therapy at home without equipment?
Absolutely. You don’t need weights or machines. Bodyweight exercises like bridges, wall sits, heel slides, and standing calf raises are powerful. Resistance bands cost under £10 and add variety. Walking, stretching, and breathing exercises require nothing. The real tool isn’t equipment-it’s consistency. Doing 10 minutes daily beats an hour once a week.
Should I use heat or ice before or after exercise?
Use heat before exercise to loosen stiff muscles-warm bath, heating pad, or warm towel for 10-15 minutes. Use ice after if you feel swelling or sharp inflammation (common after new activity). Apply ice for 15 minutes, never directly on skin. For most chronic pain without swelling, ice isn’t necessary. Focus on movement, not cold packs.
What if I don’t have time for a full routine?
Then do less-but do it every day. The Arthritis Foundation’s two-minute routine proves it: short bursts work. Do three stretches while brushing your teeth. Walk for 5 minutes after lunch. Do two bridges before bed. These micro-movements add up. You don’t need 30 minutes. You need 2 minutes, done daily. That’s how habits form.
What to Do Next
If you’re ready to move beyond painkillers, start today. Pick one exercise. Pick one stretch. Do them tomorrow. Track your pain. Notice how you feel after a week. If you’re still stuck, find a physical therapist who listens-not just one who pushes you through a checklist. The goal isn’t to suffer through exercise. It’s to move freely again. And that’s possible.

Anna Pryde-Smith
January 22, 2026 AT 13:10This is the kind of post that makes me want to scream into a pillow-because I’ve been told ‘just move more’ for YEARS, and no one ever told me HOW. I tried swimming, I tried stretching, I tried ‘micro-movements’-but when my PT said ‘do bridges’ and I did them wrong and threw out my back? Yeah. That’s not motivation. That’s a lawsuit waiting to happen. Stop glorifying ‘just do it’ like it’s a Nike ad. People aren’t broken machines. We’re traumatized nervous systems trying not to die from a 10-minute walk.
And don’t even get me started on the ‘2-hour rule.’ What if I’m a single mom working two jobs and I can’t even sit still for two hours? Who the hell are you to say my pain isn’t valid because I didn’t track it in a spreadsheet? I’m not a data point. I’m a person who cries in the shower because her knees sound like popcorn.
Stop talking about ‘restoration.’ I don’t want to be ‘restored.’ I want to be believed. And if your solution is ‘try tai chi,’ then you’re part of the problem, not the cure.
Dawson Taylor
January 23, 2026 AT 19:34While the empirical basis for physical therapy in chronic pain management is robust, the practical implementation remains fraught with systemic inefficiencies. The disjunction between clinical evidence and real-world accessibility-particularly in socioeconomic contexts where time, insurance, and provider competence are constrained-renders many of these protocols aspirational rather than actionable. One must interrogate not only the efficacy of movement-based interventions, but the epistemic authority of those who prescribe them without adequate contextual calibration.
charley lopez
January 24, 2026 AT 18:06From a biomechanical standpoint, the assertion that low-impact modalities reduce nociceptive load is well-supported by the literature. However, the generalization of exercise prescriptions-particularly the recommendation of tai chi for fibromyalgia without stratification by central sensitization profiles-risks oversimplification. The 2022 trial cited demonstrated effect sizes, but did not control for placebo response or adherence bias. Furthermore, the absence of neuromuscular recruitment metrics in home-based protocols limits reproducibility. A standardized movement analysis protocol, ideally validated via wearable inertial sensors, would significantly enhance fidelity.
Susannah Green
January 26, 2026 AT 11:20Okay, I’m gonna say this nice and slow so it sticks: YOU DON’T NEED A GYM. You don’t need a referral. You don’t need to wait until you’re ‘ready.’
Do the cat-cow while you wait for your coffee. Do two bridges before you brush your teeth. Walk around the block while you listen to your favorite podcast. That’s it. That’s the whole thing.
I had 10 years of lower back pain. I tried everything-meds, injections, acupuncture, yoga retreats in Bali (yes, really). Nothing worked until I stopped trying to ‘fix’ myself and just moved, a little, every day. No pain? Great. Pain? Okay, back off. Don’t quit. Just adjust.
And if your PT tells you to ‘push through it’? Find a new one. Pain isn’t a badge of honor. It’s a signal. Listen to it. Not your ego. Not your Instagram fitness influencer. YOU.
Start today. Not Monday. Today.
P.S. Resistance bands are $8 on Amazon. You’re welcome.
Kerry Moore
January 28, 2026 AT 09:06The integration of graded exposure principles into chronic pain rehabilitation represents a paradigmatic shift from symptom suppression to neuroplastic retraining. However, the translational gap between research findings and clinical delivery remains substantial, particularly in resource-limited settings. The cited VA study demonstrating increased adherence via video instruction is compelling, yet it raises questions regarding digital equity and cognitive load for elderly or neurodivergent populations. Further inquiry into adaptive, AI-assisted feedback systems may mitigate these disparities.
Stacy Thomes
January 28, 2026 AT 21:28I DID IT. I actually did it. I started walking 10 minutes a day. Just 10. And guess what? I slept through the night last week for the first time in 4 years. I cried. I didn’t even know I could cry from happiness anymore.
And then I did the figure-four stretch while I waited for my microwave. And then I did it again. And again. Now I do it every morning while I make my tea.
It’s not magic. It’s not a miracle. It’s just… movement. And I’m not broken. I’m just… learning how to move again.
You can do this. I’m not saying it’s easy. But I’m saying it’s possible. And you deserve to feel better. Not someday. Now.
dana torgersen
January 30, 2026 AT 02:54so like… i think the whole thing is kinda… you know… like, your body remembers pain? not like memory memory but like… cellular memory? or something? i read this thing on tumblr that said nerves get lazy and then they start yelling for no reason? and that’s why stretching helps? idk. i’m not a doctor. but i did google it. and now i do cat-cow every morning and i feel… lighter? like my spine is breathing? i don’t know how to explain it but it’s real. and also i’m not on meds anymore. and i didn’t even try that hard. just… moved. weird right? lol
Laura Rice
January 30, 2026 AT 07:20I want to say something real: you’re not alone. I’ve been there. I’ve sat on the floor crying because I couldn’t pick up my kid. I’ve lied to my boss because I couldn’t walk to the bathroom without wincing.
But I also want to say this gently: you don’t have to fix everything today. You don’t have to be perfect. You don’t have to do 10 minutes. Five is enough. Two is enough. Even one minute counts.
And if you’re scared? That’s okay. I was too. But movement doesn’t ask you to be brave. It just asks you to try. And then try again tomorrow.
You’re not broken. You’re not lazy. You’re not failing. You’re healing. And that’s enough.
I believe in you. I really do.
Sue Stone
January 31, 2026 AT 12:07My PT told me to walk. I walked. I didn’t feel better. I quit. Two years later, I tried again. This time I walked with my dog. He doesn’t care if I’m slow. He just wants to sniff the grass. Turns out, that’s the secret. Not the stretches. Not the apps. Just… walking with something that loves you unconditionally. I’m not better. But I’m not worse. And that’s a win.
Oladeji Omobolaji
January 31, 2026 AT 23:15I live in Lagos, Nigeria. No PT here. No gym. No insurance. But I have a street vendor who sells mangoes and a bench under a tree. Every morning, I sit there and do the cat-cow stretch. I walk to the market. I carry my groceries. I don’t count steps. I don’t track pain. I just move. My back doesn’t hurt as much. I don’t know why. Maybe it’s the sun. Maybe it’s the rhythm of the city. Maybe it’s just… being alive. This post made me feel seen. Thank you.