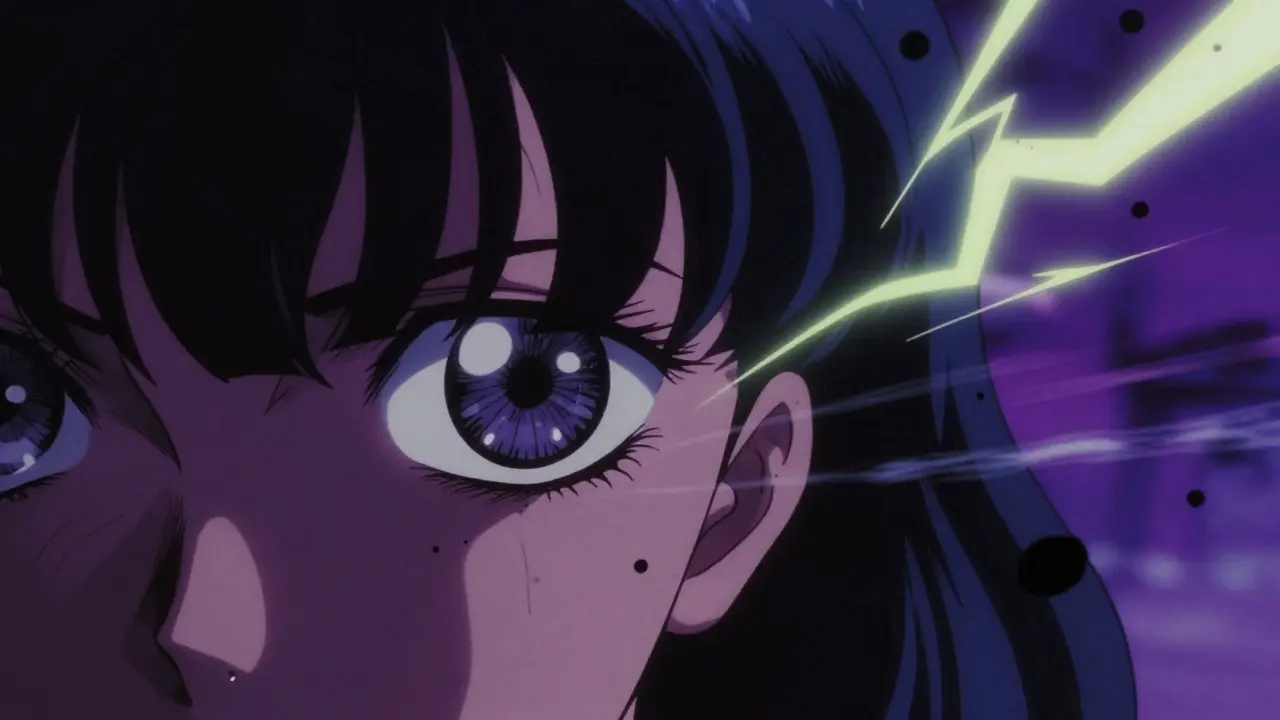
One moment your vision is clear. The next, a dark curtain is creeping across your eye. You see flashes of light like lightning in the corner of your vision. Floaters - once rare - are now everywhere, swirling like smoke. This isn’t just aging eyes. This is retinal detachment, and it’s a medical emergency that can steal your sight in hours if you wait too long.
Every year, about 28,000 people in the U.S. experience this condition. For many, it starts with something they ignore: a few new floaters, a quick flash of light. They think it’s just eye strain, fatigue, or stress. But when the retina - the thin layer of light-sensitive cells at the back of your eye - pulls away from its blood supply, time becomes the enemy. The longer you wait, the less chance you have of saving your vision. Studies show that if surgery happens within 24 hours of symptoms, there’s a 90% chance the retina can be successfully reattached. After 72 hours, your odds of regaining 20/40 vision drop from 75% to just 35%.
What Are the Warning Signs?
Retinal detachment doesn’t come with pain. That’s what makes it so dangerous. You won’t feel it. You’ll only see it - and sometimes, you won’t even notice until it’s too late. There are six key symptoms you need to recognize immediately:
- Sudden increase in floaters: Not just one or two. Dozens. Dark spots, squiggly lines, or cobwebs that appear out of nowhere and won’t go away.
- Flashes of light: Like camera flashes or streaks of lightning, especially in your peripheral vision. These aren’t just afterimages from bright lights - they’re persistent and happen in the dark, too.
- A dark shadow or curtain: This is the most urgent sign. It starts at the edge of your vision and slowly moves inward, like a curtain being pulled across a window. Once it reaches your central vision, you’re losing sight.
- Blurry or distorted vision: Everything looks foggy, warped, or out of focus - even if you’re wearing glasses. This happens in about 68% of cases.
- Loss of peripheral vision: You can’t see things out of the corner of your eye. It’s not just a blind spot - it’s a growing area of missing vision.
- Sudden color changes: Colors look washed out, dull, or different than before. This usually means the macula (the center of your retina) is affected.
If you experience even one of these - especially if they come on suddenly - don’t wait. Don’t call your primary care doctor. Don’t wait until tomorrow. Go to an eye specialist today. A general ophthalmologist might miss early signs. Retinal specialists catch them 95% of the time. General doctors miss about 22% of cases.
How Is It Diagnosed?
There’s no home test for retinal detachment. You need specialized tools and training. A routine eye exam won’t cut it. The gold standard is a dilated fundus examination. Your doctor will put drops in your eyes to widen your pupils, then use an indirect ophthalmoscope - a bright light with a special lens - to look deep into the back of your eye. They’ll check for tears, holes, or areas where the retina has lifted.
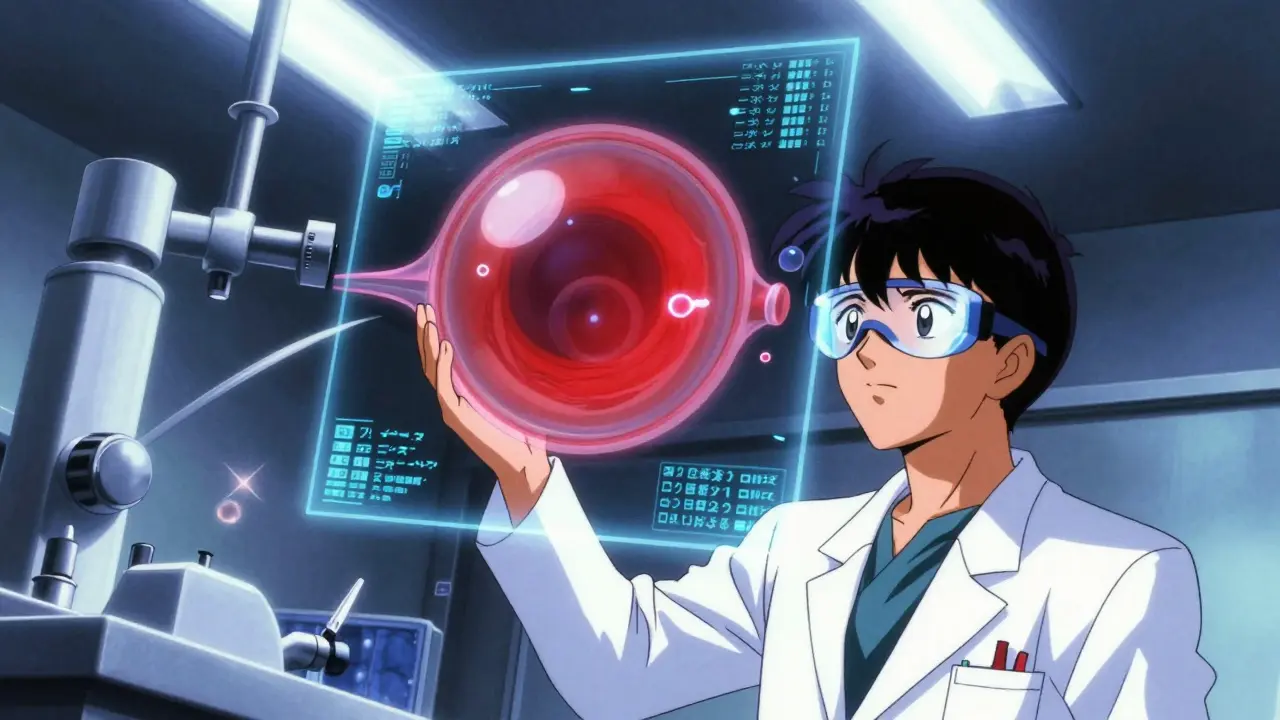
If your eye is cloudy from cataracts or bleeding, they’ll use a B-scan ultrasound. This creates a picture of the retina using sound waves, even when they can’t see it directly. For detailed imaging, they’ll use optical coherence tomography (OCT), which gives a cross-section view of the retina like a 3D map. These tools are standard in any clinic that treats retinal emergencies.
Equipment matters. You need a slit lamp, a 20D or stronger indirect ophthalmoscope, and a B-scan machine. The average cost to set up a basic diagnostic setup is over $28,500. That’s why not every clinic can handle this - and why delays happen in rural areas. Only 35% of U.S. counties have a retinal specialist nearby.
Surgical Options: What Works and When?
There are three main surgeries. The right one depends on where the detachment is, how big it is, and whether the macula is still attached.
Pneumatic Retinopexy
This is the least invasive. A gas bubble is injected into your eye. You’re then positioned so the bubble floats up and presses against the detached area, sealing the tear. A laser or freezing treatment is used to glue the retina back in place. Success rate: 70-80% for simple, superior tears.
But it only works if the tear is on the top half of the retina. If it’s below, the bubble won’t reach it. You’ll need to stay face-down or on your side for 50 of every 24 hours for 7-10 days. That’s hard. People report back pain, neck strain, and trouble sleeping. About 30% of patients need a second surgery.
Scleral Buckling
This is an older technique, but still effective. A silicone band is stitched around the outside of your eye, gently pushing the wall inward to support the retina. It’s often used for younger patients with lattice degeneration or large tears.
Success rate: 85-90%. But it comes with trade-offs. You’re likely to develop nearsightedness - 1.5 to 2.0 diopters on average. About 5-8% of patients get double vision afterward. It doesn’t speed up cataracts, which is a plus if you’re under 50 and still have your natural lens.
Vitrectomy
This is the most common surgery today - used in about 65% of cases. The surgeon removes the vitreous gel inside your eye and replaces it with a gas or silicone oil bubble. This pushes the retina back into place. Laser or freezing is used to seal tears.
Success rate: 90-95%, especially for complex cases like giant tears or when scar tissue has formed. It’s the only option if the macula is already detached. But here’s the catch: 70% of people who still have their natural lens will develop a cataract within two years. You’ll likely need cataract surgery later.
Newer versions use 27-gauge instruments - smaller cuts, less trauma. Intraoperative OCT is now used in many centers to guide the surgeon in real time, improving precision by 15%.
Who’s at Risk?
Retinal detachment can happen to anyone, but some groups are far more vulnerable:
- People over 40: Risk jumps from 1 in 10,000 to 20 in 10,000.
- Severe nearsightedness: If you’re -5.00D or worse, your risk is 167 in 10,000 - more than 15 times higher.
- After cataract surgery: 0.5-2% of patients develop detachment within 5 years.
- Lattice degeneration: A thinning of the retina seen in about 10% of people. It increases lifetime risk to 1%.
- Family history: If a close relative had it, your risk goes up.
- Eye trauma: A blow to the eye can cause tears that lead to detachment.
Some doctors debate whether to treat lattice degeneration before it causes detachment. One side says: prevent it. The other says: don’t operate unless there’s a tear. The choice depends on your specific case, age, and risk factors.
What Happens After Surgery?
Surgery isn’t the end - it’s just the beginning of recovery. If you had a gas bubble, you’ll need to keep your head in a specific position for days. Face-down. Side-lying. No lying flat. This isn’t optional. If the bubble doesn’t press against the tear, the retina won’t stick.
Many patients need help at home. Over a third require visiting nurses or family members to assist with daily tasks. Driving is off-limits until the gas bubble dissolves - which can take 2-8 weeks. You can’t fly. Even small changes in altitude can make the gas expand and damage your eye.
Complications are common. Elevated eye pressure happens in 25% of cases. Infection is rare but serious. Recurrent detachment occurs in 5-15% of patients. And as mentioned, cataracts almost always develop after vitrectomy in people who still have their natural lens.
Why Speed Matters More Than Anything
Every hour counts. Not every day. Not every week. Every hour.
One patient on Reddit ignored floaters for three days. When the curtain came, it was too late. His vision ended at 20/100. He could have had 20/25 if he’d gone in the same day.
Another study found that 63% of patients were initially told they had “eye strain” by their primary care doctor. The average delay? 48 hours. That’s two full days of photoreceptors dying.
At Wills Eye Hospital, the protocol is clear: if the macula is off, you get seen within 4 hours and operated on within 12. That’s not a suggestion - it’s standard. And patients treated within 12 hours report 92% satisfaction. After 48 hours? Only 67%.
What’s Next for Treatment?
Surgery is getting better. New tools like the EVA Platform allow smaller incisions and faster recovery. AI is being tested to spot early signs of detachment in routine eye scans - potentially cutting diagnosis delays by 30% in the next five years.
Future treatments might include bioengineered retinal patches or gene therapies for inherited conditions that weaken the retina. But right now, the best defense is knowing the signs and acting fast.
Don’t wait for a second opinion. Don’t hope it goes away. If you see flashes, a curtain, or a flood of new floaters - get to an eye specialist immediately. Your vision isn’t just blurry. It’s disappearing. And once it’s gone, you can’t get it back.
Can retinal detachment fix itself?
No. Retinal detachment cannot heal on its own. The retina needs to be physically reattached using surgery. Without treatment, the photoreceptor cells die permanently, leading to irreversible vision loss. Even small detachments will grow over time.
How long does retinal detachment surgery take?
Most procedures last between 1 and 2 hours. Pneumatic retinopexy is the quickest - often under an hour. Vitrectomy can take longer, especially if complications are present. Recovery time varies, but most people return to light activities within a week, though full healing takes weeks to months.
Is retinal detachment surgery painful?
The surgery itself is done under local or general anesthesia, so you won’t feel anything during the procedure. Afterward, most people report mild discomfort, pressure, or a scratchy feeling - not severe pain. Pain medication is usually only needed for a day or two.
Can I drive after retinal detachment surgery?
No, not until the gas bubble in your eye has completely dissolved - which can take 2 to 8 weeks. Flying is also prohibited during this time because changes in air pressure can cause the gas to expand and damage your eye. Your doctor will tell you exactly when it’s safe to drive again.
Will I need glasses after surgery?
You may. Scleral buckling often causes new nearsightedness, requiring stronger glasses. After vitrectomy, most people develop cataracts within two years, which also affects vision and usually requires lens replacement. Your prescription may change multiple times during recovery.
Can retinal detachment happen again?
Yes. About 5-15% of patients experience a recurrence, depending on the type of surgery and the original cause. People with severe myopia or lattice degeneration are at higher risk. Regular eye exams are essential - even years after surgery.
How much does retinal detachment surgery cost?
In the U.S., Medicare reimburses about $3,850 for pneumatic retinopexy and $7,200 for vitrectomy. Costs vary by location and hospital, but most private insurance covers the full procedure. Out-of-pocket costs depend on your plan’s deductible and co-pay.
What should I do if I only have one eye?
If you have vision in only one eye, any symptom of retinal detachment is an absolute emergency. Losing vision in your only seeing eye means total blindness. Seek care immediately - even if you think it might be nothing. There’s no room for delay.
Final Thought: Don’t Wait
People lose their sight from retinal detachment not because the treatment doesn’t work - but because they don’t act fast enough. The tools, the expertise, the technology - they’re all here. What’s missing is awareness.
Flashes and floaters aren’t normal. A dark curtain isn’t just a shadow. It’s your vision slipping away. If you see it - don’t wait. Don’t call your doctor tomorrow. Go now. Your eyesight is worth every minute.
Kathy Scaman
January 28, 2026 AT 04:51I saw a floater last week and panicked for three days thinking it was this. Turned out it was just a weird reflection from my phone screen. But holy crap, this post scared me into finally scheduling that annual eye exam I’ve been dodging. Thanks for the wake-up call.
Bryan Fracchia
January 28, 2026 AT 15:00It’s wild how medicine still relies so heavily on patient awareness when the tech to catch this early exists. AI screening in routine optometry visits could save thousands of eyes - but we’re still stuck in a system where you have to scream ‘I’m going blind!’ before anyone takes you seriously. We treat vision like it’s optional until it’s gone.
Timothy Davis
January 30, 2026 AT 14:50Let’s be real - 90% success rate within 24 hours? That’s a marketing stat. Real-world data from the 2022 JAMA Ophthalmology meta-analysis shows only 68% anatomical success with macula-on cases when you factor in comorbidities and rural delays. And don’t even get me started on how ‘vitreous gel removal’ is just a fancy way of saying ‘you’re gonna get cataracts in 2 years’.
Also, ‘don’t wait’? Yeah, easy to say when you’ve got a 401(k) and a retina specialist 15 minutes away. Try living in rural Alabama and seeing what happens when your PCP says ‘it’s probably allergies’.
fiona vaz
February 1, 2026 AT 12:47I’m an optician and I’ve seen this too many times. People come in with a curtain and say, ‘I thought it was just tired eyes.’ I always tell them: your eyes don’t lie - but your brain does. It wants to believe it’s nothing. Please, if you’re reading this and you’ve had sudden floaters - go. Don’t text your friend. Don’t Google it. Just go.