What Medications Actually Work for OCD?
When you're stuck in cycles of obsessive thoughts and compulsive behaviors, finding the right medication can feel like searching for a needle in a haystack. Not every antidepressant helps with OCD. In fact, only two classes of drugs have solid, proven results: SSRIs and clomipramine. These aren't just common prescriptions-they're the only treatments backed by decades of clinical research and endorsed by global mental health guidelines.
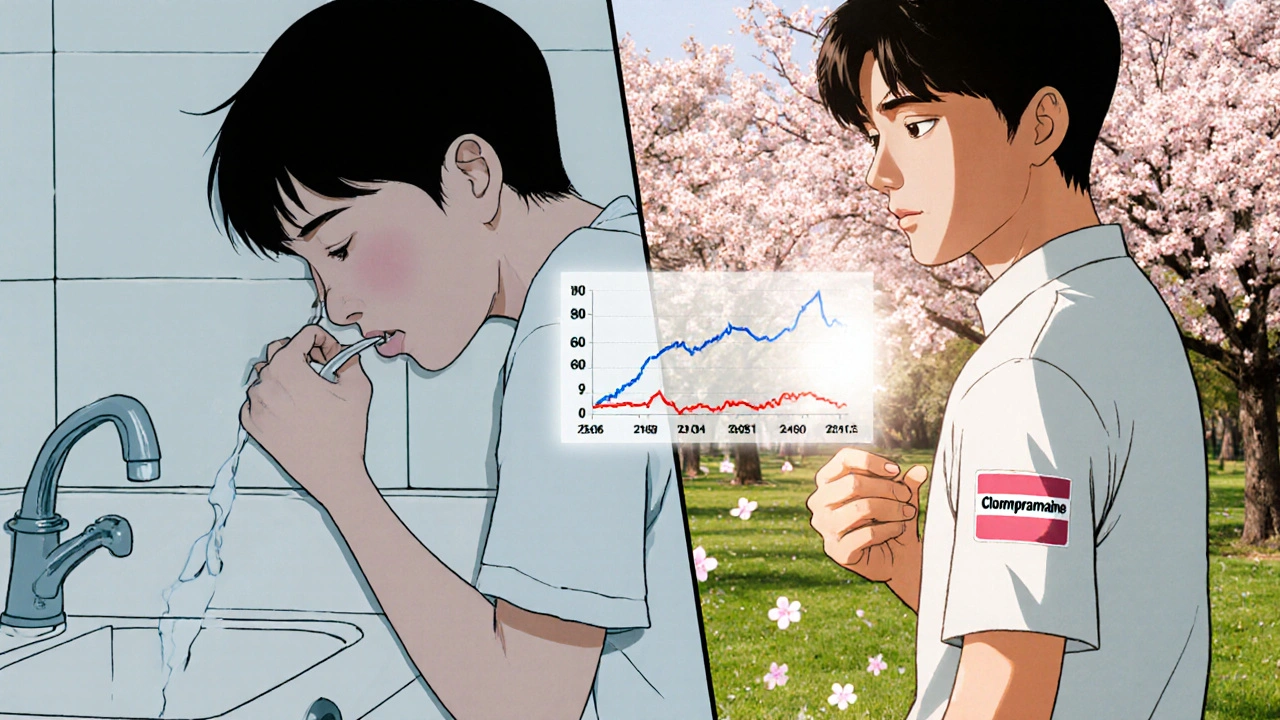
SSRIs-selective serotonin reuptake inhibitors-are the first-line choice for most people. That means doctors start here before trying anything else. Why? Because they work, and they're generally safer than older options. Clomipramine, a tricyclic antidepressant, was the first drug ever approved by the FDA specifically for OCD back in 1989. It's powerful, but it comes with more side effects. That’s why it’s usually reserved for cases where SSRIs don’t cut it.
How SSRIs Work for OCD (And Why Dosing Is Different)
Many people assume that if an SSRI works for depression, it’ll work the same way for OCD. That’s not true. The doses needed for OCD are much higher than those used for depression. A typical starting dose for depression might be 20 mg of sertraline. For OCD? You’re often looking at 50 mg or more-sometimes up to 200-300 mg.
Here’s what the standard SSRI dosing looks like for OCD:
- Fluoxetine (Prozac): Start at 20 mg, increase to 40-60 mg daily
- Fluvoxamine (Luvox): Start at 25-50 mg, go up to 200-300 mg daily
- Paroxetine (Paxil): Start at 20 mg, target 40-60 mg daily
- Sertraline (Zoloft): Start at 50 mg, often reach 200-300 mg daily
It takes time. Don’t expect results in two weeks. Most people need 8 to 12 weeks of consistent dosing at therapeutic levels before noticing real change. And even then, improvement isn’t always dramatic. A 25-35% reduction in symptoms-measured by the Yale-Brown Obsessive Compulsive Scale-is considered a good outcome. That means the rituals still happen, but they’re less intense, less frequent, and less controlling.
Clomipramine: The Old-School Option With Real Power
Clomipramine (brand name Anafranil) isn’t flashy, but it’s been around long enough to prove itself. It’s not an SSRI-it works on multiple neurotransmitters, not just serotonin. That broader action might explain why it sometimes works when SSRIs fail.
Dosing for clomipramine is precise and slow:
- Adults: Start at 25 mg daily. Increase by 25 mg every 4-7 days. Most people need 100-250 mg daily. Max is 250 mg.
- Teens (10+ years): 1-3 mg per kg of body weight, max 200-250 mg daily
- Elderly: Start at 10 mg, rarely go above 50 mg
Doctors often give clomipramine at night because it causes heavy drowsiness. Some split the dose-half in the morning, half at night-to balance side effects. Blood levels matter too. Studies show people who respond well to clomipramine typically have plasma levels between 220-350 ng/mL. That’s why some psychiatrists order blood tests after a few weeks, especially if the dose is above 150 mg.
SSRIs vs. Clomipramine: What the Data Says
It’s not a simple “which is better?” question. The answer depends on who you are.
In adults, multiple head-to-head trials show SSRIs and clomipramine are equally effective. But here’s the catch: clomipramine causes side effects 3-5 times more often. Dry mouth, blurred vision, constipation, weight gain, dizziness, and heart rhythm changes (like prolonged QTc interval) are common. One study found 28% of people quit clomipramine due to side effects, compared to just 15-18% for SSRIs.
For kids and teens? The data flips. One meta-analysis showed clomipramine improved OCD symptoms by 37% in children-more than sertraline, fluoxetine, or fluvoxamine. But because of safety concerns, doctors still usually try SSRIs first. The risk of heart issues and seizures is higher in younger patients, even if the benefit is stronger.
Clomipramine also seems to work better for specific OCD types-especially contamination fears and cleaning compulsions. At doses of 150-250 mg, it can shut down those intense urges in ways SSRIs sometimes can’t.
What Patients Actually Experience
Real-world stories don’t always match clinical trials.
On Reddit’s r/OCD community, 78% of users who tried clomipramine said they only felt real relief at 150 mg or higher. But 43% stopped because of side effects. One user wrote: “Clomipramine at 175 mg finally stopped my checking rituals after 5 failed SSRIs. But I was so tired I couldn’t work. I switched back to sertraline-better, but not perfect.”
On forums like OCD-UK, 62% of 1,247 respondents said SSRIs were easier to tolerate. Common complaints about clomipramine? “I drank 5-6 glasses of water an hour just to stop my mouth from drying out.” “I gained 20 pounds in six months.” “I felt like I was walking through syrup.”
Still, on Drugs.com, clomipramine has a slightly higher effectiveness rating (7.2/10) than SSRIs (6.8/10). But satisfaction? Clomipramine scores 5.1/10. SSRIs get 6.2/10. The trade-off is clear: clomipramine can work better-but it costs more in daily discomfort.
When and How Doctors Decide
Psychiatrists follow a clear roadmap:
- Start with an SSRI at a high dose. Wait 8-12 weeks.
- If there’s no improvement, switch to another SSRI. Wait another 8-12 weeks.
- If still no response, consider clomipramine-or add a low dose of clomipramine (25-75 mg) to an ongoing SSRI. This “augmentation” strategy works for 35-40% of people who only partially responded to SSRIs.
Before starting clomipramine, doctors usually order an ECG to check heart rhythm. Liver function tests are common too. And they’ll monitor weight, blood pressure, and symptoms closely. If you’re on more than 150 mg of clomipramine, regular blood tests are often recommended.
Many patients panic in the first two weeks. OCD symptoms can get worse before they get better. That’s normal. About 37% of people consider quitting during this phase. But 89% of those who stick it out see improvement within 4-6 weeks. That’s why psychoeducation matters-knowing this is temporary can save your treatment.
What’s Coming Next
The field is changing. In March 2023, the FDA gave Breakthrough Therapy status to a new drug called SEP-363856. Early trials showed a 45% response rate in people who didn’t respond to anything else. That’s huge.
Researchers are also testing psilocybin-yes, the active ingredient in magic mushrooms-combined with therapy and SSRIs. Early results show 60% of participants reached remission after six months, compared to 35% with SSRIs alone.
Even clomipramine is getting an upgrade. A new skin patch version is in phase 2 trials. It delivers the drug slowly, avoiding the high blood spikes that cause side effects. Early data shows the same effectiveness at 150 mg patch vs. 200 mg pill-with 40% fewer dry mouth and drowsiness complaints.
By 2028, analysts predict SSRIs will still make up 75-80% of OCD prescriptions. But clomipramine’s role will shift: not as a first try, but as a targeted tool for severe, stubborn cases.
What You Should Do Next
If you’re on an SSRI and not improving after 12 weeks at a high dose, talk to your doctor about switching or adding clomipramine. Don’t wait. OCD thrives in silence and delay.
If you’re considering clomipramine, ask for a baseline ECG. Ask about blood tests. Ask how they’ll monitor your heart and liver. Don’t be afraid to push for a slow titration-starting at 12.5 mg instead of 25 mg can make a big difference in tolerability.
And remember: medication alone rarely cures OCD. It makes therapy possible. Exposure and Response Prevention (ERP) is the gold-standard therapy. Medication helps you get through the anxiety to do the work. Together, they’re the most powerful combo you’ve got.
Can SSRIs make OCD worse at first?
Yes, it’s common. In the first 1-2 weeks, OCD symptoms can temporarily spike. This happens in about 37% of cases. But if you keep taking the medication, symptoms improve in 89% of people by week 4-6. Your doctor should warn you about this upfront. Don’t stop-talk to them instead.
Is clomipramine safe for teenagers?
Yes, but with caution. Clomipramine is FDA-approved for kids 10 and older. Dosing is based on weight (1-3 mg per kg), with a max of 200-250 mg daily. Doctors usually start low-25 mg or less-and go slow. Heart monitoring (ECG) is required before and during treatment because of risks like QTc prolongation. It’s effective, but SSRIs are still tried first due to safety.
Why is clomipramine not used more often?
Because of side effects. Clomipramine causes dry mouth, drowsiness, weight gain, constipation, blurred vision, and heart rhythm changes at much higher rates than SSRIs. About 28% of people stop taking it because of these issues, compared to 15-18% for SSRIs. Even though it works well-especially for severe cases-the risks make doctors hesitant to start with it.
How long does it take for OCD meds to work?
At least 8-12 weeks. Unlike anxiety meds like benzos, SSRIs and clomipramine don’t work fast. Most people don’t notice improvement until after 6 weeks of being on a full therapeutic dose. Patience is critical. Stopping too soon means you’ll never know if it could have helped.
Can I take clomipramine with an SSRI?
Yes-this is called augmentation. If you’re on an SSRI but only improving partially, adding a low dose of clomipramine (25-75 mg/day) can boost results. About 35-40% of people who don’t respond fully to SSRIs see meaningful improvement with this combo. But it increases side effect risk, so it’s only done under close medical supervision.
Are there cheaper alternatives to brand-name OCD meds?
Yes. All the main SSRIs (sertraline, fluoxetine, paroxetine) and clomipramine are available as generics. Generic sertraline costs about $10-$20 per month. Clomipramine generics run $50-$100 monthly, depending on dose and pharmacy. Brand names like Luvox or Anafranil can cost $300-$600. Always ask your pharmacist for the generic version unless there’s a medical reason not to.

ASHISH TURAN
November 14, 2025 AT 11:30Ryan Airey
November 15, 2025 AT 03:17Hollis Hollywood
November 15, 2025 AT 11:27Aidan McCord-Amasis
November 17, 2025 AT 09:41Shyamal Spadoni
November 17, 2025 AT 16:44Ogonna Igbo
November 19, 2025 AT 10:44BABA SABKA
November 20, 2025 AT 19:19Chris Bryan
November 22, 2025 AT 02:31Jonathan Dobey
November 23, 2025 AT 21:20