When you're on a DOAC - whether it's apixaban, rivaroxaban, dabigatran, edoxaban, or betrixaban - you're taking a blood thinner designed to prevent clots without the hassle of regular blood tests. That’s the big sell. But here’s the catch: even though DOACs are simpler than warfarin, they don’t play nice with every other medication you might be taking. And if you're over 65, which most DOAC patients are, you're probably on five or more other pills. That’s not rare - it’s normal. And that’s where things get risky.
How DOACs Work - and Why Interactions Matter
DOACs work by blocking specific proteins in your blood that help clots form. Unlike warfarin, which needs constant monitoring and is affected by vitamin K in your diet, DOACs have a more predictable effect. But their predictability depends on one thing: your blood levels. If something changes how much of the drug gets into your bloodstream - either by blocking its absorption or speeding up its breakdown - your risk of bleeding or clotting goes up.
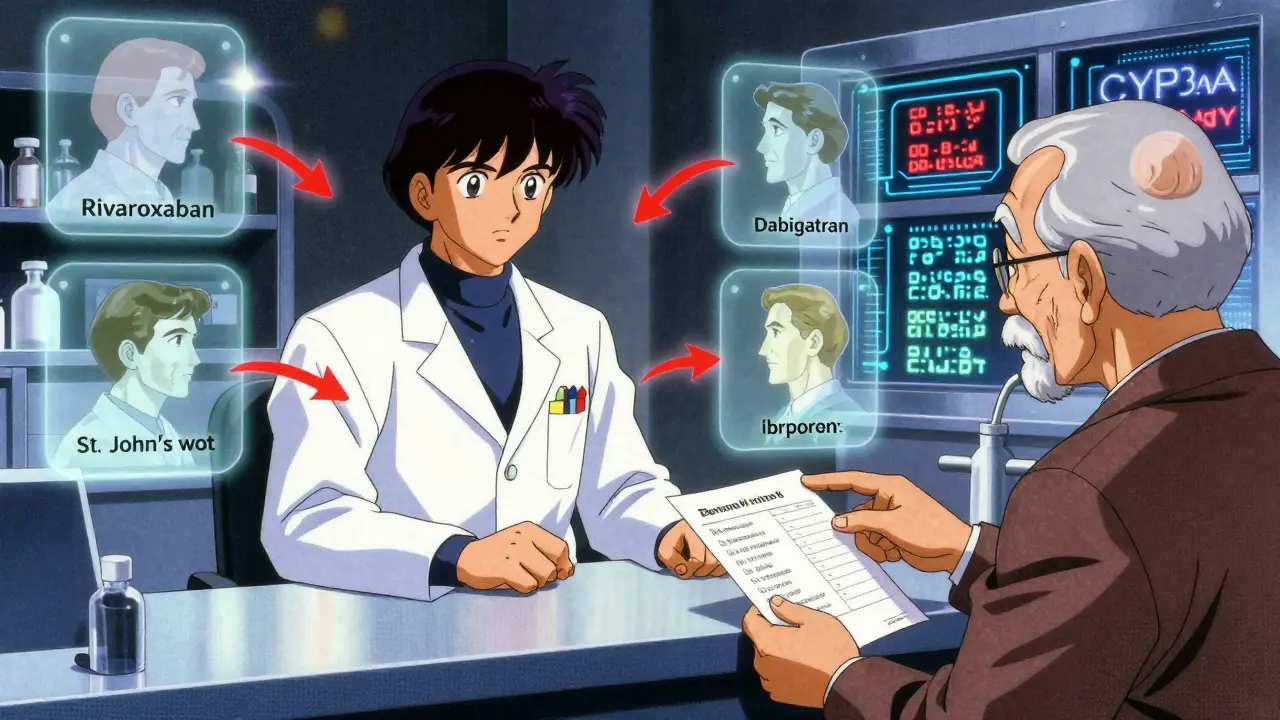
Two main systems control how DOACs move through your body: the CYP3A4 enzyme and the P-gp transporter. Think of them like gatekeepers. If a drug shuts down these gatekeepers (inhibitor), your DOAC builds up. Too much? Bleeding risk. If a drug opens them wide (inducer), your DOAC gets flushed out. Too little? Clot risk.
Big Red Flags: Drugs That Interact Strongly
Not all drug interactions are created equal. Some are harmless. Others can land you in the ER. Here’s what to watch for:
- Dronedarone (used for irregular heartbeat): This one’s dangerous. It strongly blocks P-gp. If you're on dabigatran or rivaroxaban, don’t take them together. It can spike DOAC levels by 2-3 times. For edoxaban, reduce the dose to 30 mg daily. Apixaban and betrixaban are safer, but still monitor closely.
- Amiodarone: Another heart rhythm drug. It moderately blocks P-gp. Mixing it with any DOAC increases bleeding risk, especially in older adults. Watch for bruising, dark stools, or unexplained fatigue.
- Diltiazem and Verapamil: These calcium channel blockers are common for high blood pressure. Diltiazem weakly blocks both CYP3A4 and P-gp. Verapamil blocks P-gp. For dabigatran, reduce the dose to 110 mg twice daily if you’re taking verapamil. For apixaban and rivaroxaban, the interaction is usually not clinically significant - but don’t assume. Check with your pharmacist.
- Strong CYP3A4 or P-gp inducers: These include rifampin, St. John’s wort, carbamazepine, and phenytoin. They can slash your DOAC levels by 50% or more. Avoid them entirely. There’s no safe dose adjustment.
It’s Not Just Prescription Drugs
Many people forget about supplements. St. John’s wort isn’t just a herbal remedy - it’s a powerful inducer. It can make your DOAC useless. Turmeric? Curcumin might interfere with platelet function. Ginkgo biloba? Increases bleeding risk. Omega-3s? High doses (over 3 grams daily) can add to the anticoagulant effect. Even common painkillers like ibuprofen or naproxen can increase bleeding risk when taken with DOACs - not because they change drug levels, but because they irritate your stomach lining and thin platelets. Same with SSRIs like fluoxetine or sertraline. They don’t touch DOAC metabolism, but they make bleeding more likely.
Differences Between DOACs - Not All Are Equal
Some people think all DOACs are the same. They’re not. Each has its own interaction profile:
| DOAC | Main Metabolic Pathway | High-Risk Interactions | Lower-Risk Interactions |
|---|---|---|---|
| Apixaban | CYP3A4 (20-25%), P-gp | Dronedarone, strong inducers | Verapamil, diltiazem (usually safe) |
| Rivaroxaban | CYP3A4 (50%), P-gp | Dronedarone, rifampin, St. John’s wort | Verapamil (low risk) |
| Dabigatran | P-gp (mainly) | Dronedarone, verapamil (dose reduction needed), amiodarone | Apixaban (less interaction risk) |
| Edoxaban | P-gp | Dronedarone (dose reduce to 30 mg), strong inducers | Apixaban, rivaroxaban (different profiles) |
For example, if you’re on rivaroxaban 20 mg once a day for atrial fibrillation, and your doctor adds diltiazem, you’re probably fine. But if you’re on rivaroxaban 2.5 mg twice daily after a heart attack, that same combo could be riskier because your baseline levels are already lower. The same drug, different dose, different risk.
What About Kidney Function?
Most DOACs are cleared by your kidneys. If your kidney function drops - and it often does with age - your doctor already lowers your dose. But here’s the problem: if you take a drug that also slows DOAC clearance (like amiodarone), you’re doubling down on risk. A 75-year-old on apixaban 5 mg twice daily with mild kidney impairment who starts amiodarone might need to drop to 2.5 mg. But no one checks that automatically. You have to ask.

What to Do - Practical Steps
Don’t panic. Just be smart. Here’s what works:
- Keep a full list of every pill, patch, capsule, and supplement you take. Include vitamins, herbs, and over-the-counter painkillers.
- Bring it to every appointment - not just your cardiologist, but your GP, pharmacist, and any specialist.
- Ask your pharmacist every time a new drug is prescribed. Pharmacists are trained to spot interactions. They see dozens of these cases a day.
- Watch for signs of bleeding: Unusual bruising, nosebleeds that won’t stop, pink or brown urine, black or tarry stools, headaches with no cause, dizziness.
- Don’t stop or change your DOAC on your own. Even if you think a new drug is harmless, don’t adjust the dose. Call your doctor.
When to Be Extra Careful
Some situations need extra attention:
- Before surgery: Even minor procedures like dental extractions or colonoscopies need planning. Your DOAC might need to pause - but not always. Guidelines vary by procedure and bleeding risk.
- During illness: Diarrhea or vomiting can reduce DOAC absorption. Fever or infection can change how your liver and kidneys work. These aren’t interactions, but they change how your body handles the drug.
- Switching between DOACs: If your doctor switches you from rivaroxaban to apixaban, don’t assume the dose is the same. They’re not interchangeable by milligram.
The Bottom Line
DOACs are safer than warfarin - but not risk-free. Their biggest advantage - fewer food and drug interactions - shouldn’t make you complacent. Polypharmacy is the norm, not the exception. And the interactions that do exist? They can be deadly.
The key isn’t avoiding every possible combo. It’s knowing which ones matter, asking the right questions, and staying involved in your own care. If you’re on a DOAC and start a new medication - even something as simple as a new painkiller - pause. Don’t just take it. Ask: Could this change how my blood thinner works?
There’s no magic tool that catches every interaction. No app is perfect. No algorithm knows your full history. But a pharmacist with your medication list? That’s your best defense.
Can I take ibuprofen with a DOAC?
It’s not recommended. Ibuprofen and other NSAIDs don’t change DOAC levels, but they increase bleeding risk by irritating the stomach lining and affecting platelets. If you need pain relief, acetaminophen (paracetamol) is safer. Always check with your doctor before using NSAIDs long-term.
Is there a blood test to check DOAC levels?
Routine blood tests like INR don’t work for DOACs. Specialized tests (anti-Xa for apixaban/rivaroxaban/edoxaban, ecarin clotting time for dabigatran) can measure levels, but they’re not standard. They’re used in emergencies, like bleeding or before surgery, or in research. Most people don’t need them.
What if I forget to take my DOAC?
If you miss a dose and remember within 6 hours, take it right away. If it’s been longer, skip it. Don’t double the next dose. For twice-daily DOACs (apixaban, dabigatran), if you miss a dose, take it only if it’s within 6 hours. For once-daily (rivaroxaban, edoxaban), if you miss it, take it as soon as you remember - but only if it’s the same day. Never double up.
Do DOACs interact with alcohol?
Moderate alcohol (1-2 drinks per day) is generally safe. Heavy drinking increases bleeding risk and can damage your liver, which affects how DOACs are processed. If you drink regularly, talk to your doctor. Binge drinking is dangerous.
Can I switch from warfarin to a DOAC safely?
Yes, but it must be done carefully. Your doctor will stop warfarin and wait for your INR to drop below 2.0 before starting the DOAC. Never overlap them unless under strict supervision. The timing matters - too early, and you risk bleeding; too late, and you risk clotting.
Are DOACs safe for people with kidney disease?
They can be, but doses are adjusted based on kidney function. Apixaban is often preferred in moderate kidney impairment because it’s partly cleared by the liver. Dabigatran is cleared mostly by the kidneys, so it’s avoided in severe kidney disease. Always have your kidney function checked before starting and annually after.

Henry Ip
January 16, 2026 AT 23:49I’ve been on apixaban for AFib for 3 years and my pharmacist caught a dangerous combo with my new antifungal script before I even filled it. Seriously, pharmacists are the unsung heroes of this game. Don’t skip the med review.
Nicholas Gabriel
January 18, 2026 AT 16:13Let me be very clear: if you're taking a DOAC, and you're over 65, and you're on more than five medications-you are in a minefield. Every pill, every supplement, every OTC painkiller-it’s not just a risk, it’s a ticking time bomb. Don’t assume it’s fine. Ask. Twice. Then ask again.
Nick Cole
January 20, 2026 AT 05:59My dad had a GI bleed last year because he started taking naproxen for his arthritis. He thought it was ‘just a painkiller.’ No one told him it could turn his DOAC into a death sentence. This post? Lifesaving. Share it with your family.
Riya Katyal
January 21, 2026 AT 18:17Oh wow, so you’re telling me that my ‘natural’ turmeric capsules aren’t just helping my inflammation… they’re also helping my blood turn into soup? Thanks, I guess I’ll just start drinking bleach instead.
Cheryl Griffith
January 22, 2026 AT 21:00I love how this post breaks it down without scaremongering. My mom’s on dabigatran and diltiazem, and her doctor actually adjusted her dose after we brought up the interaction. It’s not complicated-just requires you to show up and ask. And yes, bring your whole pill bottle. Even the gummy vitamins.
kanchan tiwari
January 24, 2026 AT 07:03THEY KNOW. They ALL KNOW. Big Pharma doesn’t want you to know how dangerous these DOACs are because they’re profitable. They’re designed to make you dependent. Your pharmacist? Paid by the pharmacy chain. Your doctor? Rushed and incentivized. They don’t care if you bleed out-they just want your refill. St. John’s wort? It’s a warning sign. The real warning? The system itself.
Bobbi-Marie Nova
January 24, 2026 AT 07:16So basically… if you’re on a DOAC, you’re basically playing Jenga with your life and someone keeps handing you new blocks labeled ‘ibuprofen’ and ‘ginkgo’? Cool. I’ll just take my tea and my acetaminophen and quietly go about my day. 😌
Ryan Hutchison
January 26, 2026 AT 06:55Why are we even using these fancy new drugs? In America, we used to just use warfarin and people lived fine. Now we got all these interactions, all these ‘special tests,’ all this confusion. Back in my day, you took your pill, you got your INR, you lived. Simple. Efficient. No magic potions. Just science.
Samyak Shertok
January 28, 2026 AT 06:40Isn’t it ironic? We’re told to trust science, yet the science is contradictory. One study says dabigatran’s safe with verapamil, another says it’s a death sentence. Who’s the real expert? The one who published? Or the one who survived? Maybe the truth is… we’re all just guessing, and the pills are just lucky charms with side effects.
Stephen Tulloch
January 29, 2026 AT 08:31Bro, I’m on rivaroxaban and I take CBD oil daily. My ‘holistic’ doc said it’s fine. But then I read this and now I’m sweating. 🤯 Is it a CYP3A4 inducer? Or inhibitor? I don’t even know anymore. I think I need to go live in the woods. 🌲🪵
Joie Cregin
January 30, 2026 AT 12:18My aunt just started on edoxaban and she’s 82. She takes 12 pills a day, including that ‘miracle’ turmeric extract from the yoga studio. I sat her down with her med list, a highlighter, and a glass of wine. We marked the red flags. She cried. Then she thanked me. This stuff matters. Not because it’s scary-it’s because it’s personal.
Melodie Lesesne
January 31, 2026 AT 20:32My grandma forgot her DOAC once and panicked for two days. Then she doubled up the next day and ended up in the ER. This post saved us. Seriously. I printed it out and taped it to her fridge next to her pill organizer. Simple. Clear. No jargon. Just facts.
brooke wright
January 31, 2026 AT 21:32Wait-so if I take a naproxen for my headache and my DOAC for my AFib, I’m basically asking for a stroke AND a bleed? And my doctor just shrugged and said ‘it’s fine’? 🤡