Medication Safety Risk Calculator
This tool calculates your personalized risk of medication side effects based on your medical history and current medications. Your data is not stored or shared.
Risk Factors Analysis
What to do next:
- Keep a detailed medication list
- Discuss your risk factors with your doctor
- Ask about medication reviews
- Consider pharmacogenomic testing if you've had unexplained side effects
When you take a new medication, your doctor doesn’t just look at your current symptoms. They’re digging into your past-your full medical history-because what happened to you before can make a drug that’s safe for others dangerous for you. It’s not guesswork. It’s science. And the numbers don’t lie.
Why Your Past Matters More Than You Think
Think of your body like a machine with a unique repair history. If you’ve had kidney disease, liver problems, or even a past allergic reaction, your body processes drugs differently. That’s why a pill that works fine for someone else might send you to the ER. According to the Merck Manual a leading clinical reference used by doctors worldwide, your medical history can change how much of a drug stays in your system-sometimes by 30% to over 500%. That’s not a small tweak. That’s a life-or-death difference.
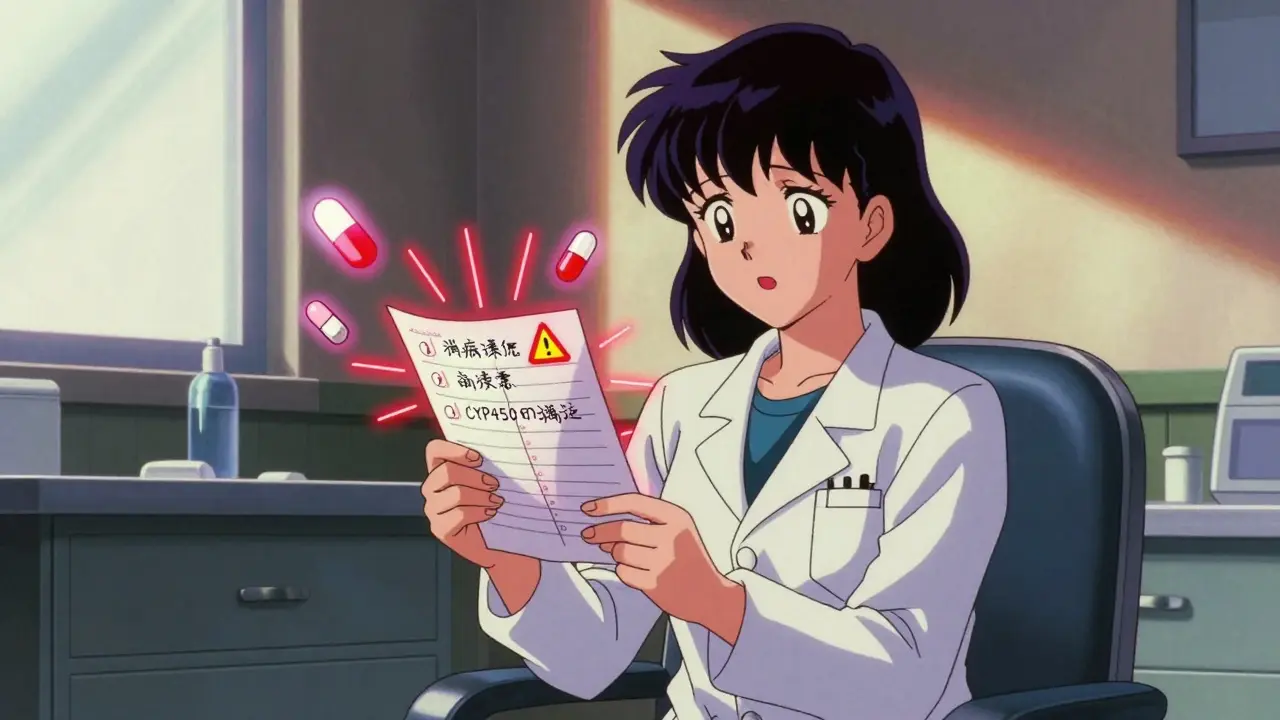
Take genetics. Some people inherit a version of the CYP450 enzyme that breaks down drugs too slowly. If you’re one of them, even a normal dose of a common painkiller or antidepressant can build up to toxic levels. You might not know you have this until you have a bad reaction. That’s why knowing your family’s drug history matters. If your mom had a severe reaction to a certain class of meds, you could be at higher risk too.
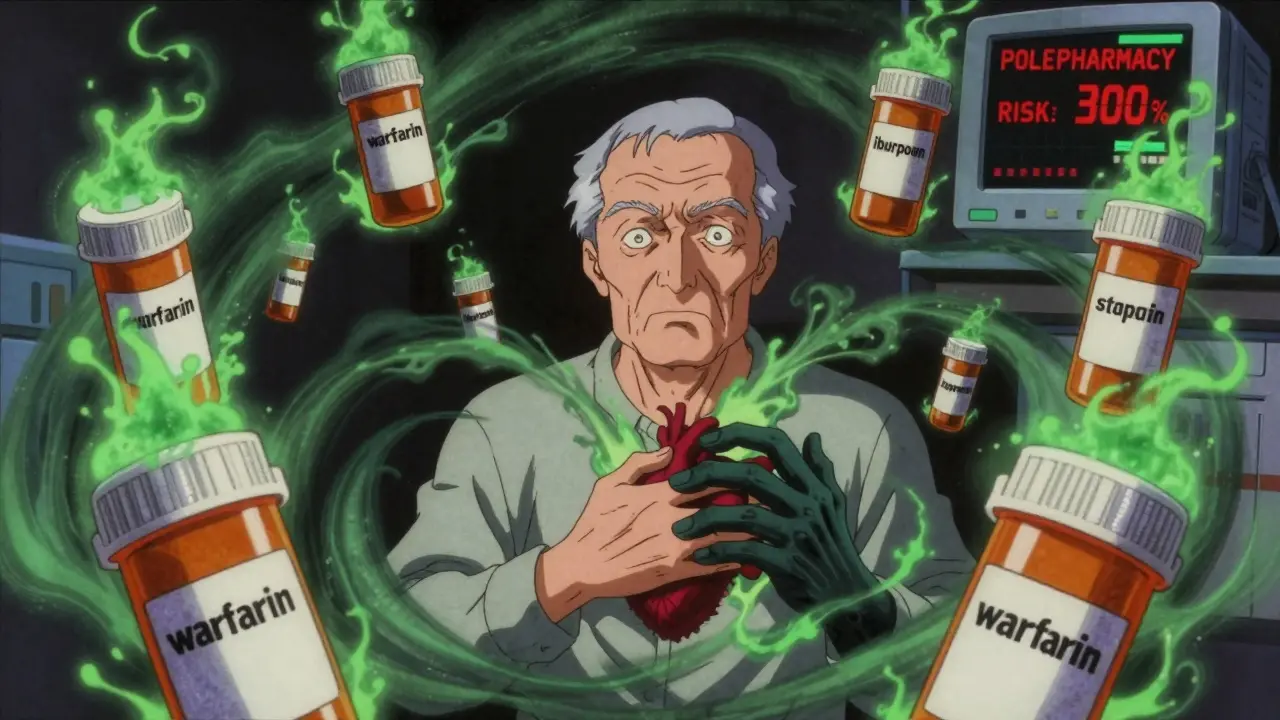
Polypharmacy: The Silent Killer
Taking five or more medications? You’re doubling your risk of a dangerous side effect. Taking ten or more? That risk jumps over three times. This isn’t theory. It’s from the British Heart Foundation 2023 analysis of real patient data. Each extra pill adds 7-10% more risk. Why? Because drugs interact-not just with diseases, but with each other.
Imagine you’re on warfarin to thin your blood, and you start taking ibuprofen for arthritis. Both are common. But together, they can cause internal bleeding. The CDC reports 34,000 emergency visits in the U.S. each year from just this one combination. And it’s not just warfarin. NSAIDs, statins, diabetes meds, antidepressants-all can clash in ways that aren’t obvious unless someone looks at your full list.
And here’s the scary part: Johns Hopkins found that only 35% of electronic prescriptions even flag known high-risk histories. Your doctor might not see that you had kidney failure five years ago. Or that you had a bad reaction to penicillin back in college. If it’s not in the system, it’s as if it never happened.
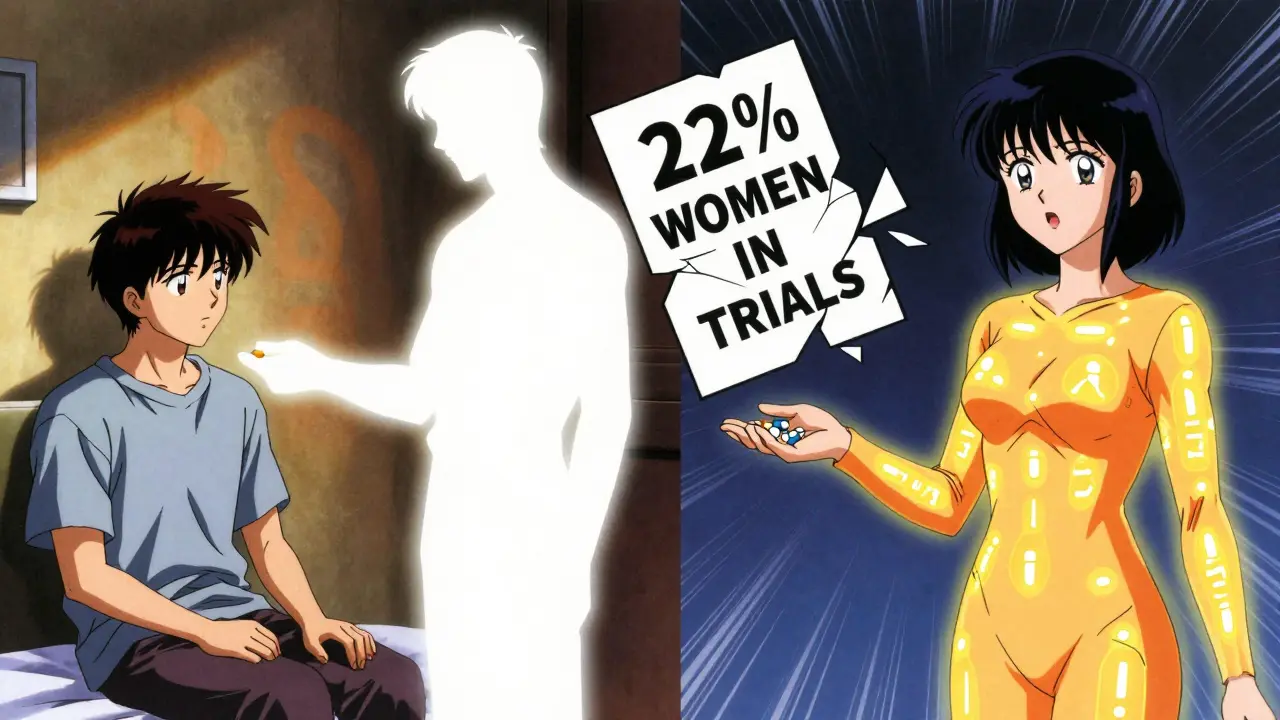
Age, Gender, and Hidden Biases
If you’re over 65, you’re 3 to 5 times more likely to have a serious side effect than someone younger. That’s not because aging makes you fragile-it’s because your liver and kidneys don’t process drugs the same way. Your body holds onto more of the drug, and clears less of it. The American Geriatrics Society 2022 data shows this clearly. Yet, many doctors still prescribe the same doses they would to a 40-year-old.
And if you’re a woman? You’re at higher risk too. Older women experience at least 50% more adverse reactions than men. Why? Because for decades, clinical trials mostly used men. Between 2010 and 2020, only 22% of participants in heart drug studies were women. So the dosing guidelines? Built for men. Your body size, hormone levels, and metabolism are different. A dose that’s safe for a man might be too strong for you. And no one told you.
Chronic Conditions Multiply the Risk
Having one chronic illness is risky. Having three or more? That’s a recipe for disaster. The Rasool et al. 2020 study in South Punjab found patients with multiple conditions had 2.6 times higher odds of medication errors. Why? Because each condition changes how drugs behave.
For example, if you have chronic kidney disease, your body can’t flush out certain drugs. The American Medical Association says 40% of commonly prescribed meds need dose adjustments for these patients. But a 2021 audit in JAMA Internal Medicine found that in nearly half of cases, doctors didn’t adjust the dose at all. You’re getting the same amount of drug as someone with healthy kidneys. That’s not a mistake. That’s a danger.
And if you have liver disease? One in four common drugs needs a dose change. But again, the system doesn’t always remind doctors. Even when the data is right there in your chart.
History of Allergies and Cross-Reactions
Think you’re safe if you only had one bad reaction? Think again. If you’re allergic to penicillin, you’re eight times more likely to react to cephalosporins-even though they’re different drugs. Why? Because they share similar chemical structures. This is called cross-reactivity.
The 2009 BMC Family Practice study found patients with a past adverse reaction to one drug class had a 30-40% higher chance of reacting to another in the same family. So if you got a rash from one antibiotic, don’t assume the next one is fine. Your immune system remembers. And it’s not always obvious. That’s why doctors now ask: "Have you ever had a reaction to ANY drug?" Not just the one you’re on.
Nonadherence Creates Its Own Danger
Skipping doses because the meds cost too much? You’re not just risking your health-you’re making side effects more likely. The American Medical Association reports 25% of patients skip doses due to cost. But when you restart after going off, your body doesn’t know how to handle it. You might get a sudden spike in drug levels, triggering dizziness, nausea, or worse.
A 2022 study of over 12,000 Medicare patients showed that those who skipped doses had 28% more side effects when they restarted. And 37% more treatment failures. That means your condition gets worse, so your doctor prescribes more drugs-which makes the cycle worse. It’s a trap.
What You Can Do
You can’t control your past. But you can control how it’s used. Here’s what works:
- Keep a written list of every medication you’ve ever taken-even over-the-counter ones, supplements, and herbal remedies. Include the dose and why you stopped.
- Bring it to every appointment. Don’t assume your doctor has it. Most don’t.
- Ask: "Could this drug interact with my past conditions?" Or: "Could my history of kidney disease change how this works?"
- Request a medication review. The Cochrane Review found structured reviews reduce side effects by 22%. But only 18% of eligible patients get them.
- Know your genetic risks. If you’ve had unexplained side effects, ask about pharmacogenomic testing. Platforms like YouScript analyze 27 gene-drug interactions and can cut side effects by 34%. But it’s still rare-only 5.7% of U.S. clinics offer it.
Why This Isn’t Just a "Doctor’s Problem"
Patients often don’t realize that side effects like confusion, fatigue, or dizziness might be from a drug-not their disease. The Merck Manual warns that medications can mimic illness. A beta-blocker can hide the fast heartbeat of internal bleeding. Steroids can mask pain from a perforated ulcer. If your doctor doesn’t know your full history, they’ll treat the symptom, not the cause.
And here’s the truth: 62% of people with chronic conditions say their providers didn’t recognize their side effects as drug-related. Why? Because the history wasn’t connected. Your past isn’t just background. It’s part of the diagnosis.
Every pill you take is a conversation between your body and the drug. Your medical history is the voice that tells the drug how to behave. If that voice isn’t heard, the result isn’t just a side effect-it’s harm you didn’t have to suffer.
Can my past allergic reaction affect new medications?
Yes. If you’ve had an allergic reaction to one drug, especially in the same class (like penicillin), you’re at higher risk of reacting to similar drugs. For example, a penicillin allergy increases the chance of reacting to cephalosporins by up to 8 times. Always tell your doctor about any past reaction, even if it was years ago.
Why do older adults have more side effects?
As we age, our liver and kidneys process drugs more slowly. This means medications stay in the body longer, increasing the chance of buildup and toxicity. People over 65 experience 3 to 5 times more adverse reactions than younger adults, even at standard doses. Dose adjustments are often needed but frequently missed.
Does gender affect how drugs work?
Yes. Women, especially older women, experience at least 50% more adverse drug reactions than men. This is partly because clinical trials historically used mostly male participants, so dosing guidelines were designed for male physiology. Women often have different body fat, hormone levels, and enzyme activity, which affect how drugs are absorbed and broken down.
What is polypharmacy, and why is it dangerous?
Polypharmacy means taking five or more medications at once. Each additional drug increases your risk of a side effect by 7-10%. With 10 or more medications, the risk triples. The danger comes from drug-drug interactions, overlapping side effects, and the body’s reduced ability to clear drugs, especially in older or chronically ill patients.
Can skipping doses make side effects worse?
Yes. Skipping doses, especially due to cost, can lead to treatment failure and higher side effect risk when you restart. Your body doesn’t adjust gradually, so drug levels can spike suddenly. Studies show people who skip doses have 28% more side effects when they restart medication compared to those who take it consistently.
Should I ask for genetic testing before taking new meds?
If you’ve had unexplained side effects, or if you’re on multiple medications, genetic testing can help. Platforms like YouScript analyze how your genes affect drug metabolism and can reduce side effects by up to 34%. While not yet widely available, it’s worth asking your doctor if you’re at high risk.
How can I make sure my doctor knows my full history?
Keep a written, up-to-date list of all medications-prescription, over-the-counter, supplements, and herbal products. Include doses, dates started/stopped, and any side effects. Bring it to every appointment. Ask: "Did you see that I had kidney disease in 2021?" or "Could this interact with my past reaction to penicillin?" Don’t assume they’ll find it in your records.
Final Thought: Your History Is Your Shield
Medical history isn’t just a record. It’s your early warning system. The more complete it is, the safer your treatment will be. You’re not just a patient. You’re the expert on your own body. Speak up. Bring your list. Ask the hard questions. Because when it comes to medications, your past doesn’t just matter-it could save your life.
Rachidi Toupé GAGNON
February 13, 2026 AT 16:02Wow. This hit different. 🤯 I’ve been on 7 meds and never realized my kidney issue from 5 years ago was silently turning my painkillers into poison. Thanks for laying it out like a comic book-clear, punchy, and real.
Bring the list. Write it down. Tell your doc. Do it now. Your future self will high-five you. ✅
Jim Johnson
February 15, 2026 AT 14:28man i used to think my dizziness was just aging, turns out it was my doctor giving me the same dose as a 30yo guy. 😅
now i carry a folded paper in my wallet with every drug i’ve ever taken. even that one time i took ibuprofen for a headache in 2017. yep. included.
you’re not being paranoid-you’re being smart. keep it up, fam.
Vamsi Krishna
February 15, 2026 AT 22:42Actually, you’re all missing the real issue. It’s not just your history-it’s the *system*. Doctors don’t have time. EHRs are garbage. Pharmacists? Overworked. And don’t get me started on how insurance companies block genetic testing unless you’re literally dying.
And yet you’re all acting like this is a personal responsibility issue? Nah. This is a structural failure. Your list? Cute. But the system ain’t gonna change because you brought a piece of paper. It’s gonna change when we sue the hell out of these hospitals and drug companies.
…I’m not mad. I’m just disappointed. And I’ve got 3 lawsuits pending.
Sophia Nelson
February 17, 2026 AT 03:08So… you’re telling me I’m supposed to memorize every drug I’ve ever taken since 2003? And bring it to every appointment? Like a homework assignment? 😑
My doctor barely looks up from his screen. He doesn’t even ask. Why should I?
Skilken Awe
February 17, 2026 AT 07:21LMAO. "Bring your list." Yeah, right. Like the 70-year-old woman with dementia and 12 meds is gonna do that. Or the guy on Medicaid who can’t afford a printer. This post reads like a corporate wellness pamphlet written by someone who’s never met a real patient.
Meanwhile, the CDC says 80% of drug errors happen because the chart is outdated. So… who’s responsible? The patient? Or the $2 billion EHR industry that built a system no one can use?
Stop victim-blaming. Fix the tech.
steve sunio
February 18, 2026 AT 22:54bro this is so true but like… why do we even have to do this? I mean, im from nigeria and here if u go to clinic, they just give u pills without even asking ur history. but here in usa u gotta be a detective just to not die? this is messed up.
also i think ur stats are fake. like 500%? that sounds like ai wrote this. 😴
Neha Motiwala
February 20, 2026 AT 05:24I knew it. I KNEW IT. This is all part of the pharmaceutical agenda. They don’t want us to know how our bodies work-they want us dependent. That’s why they don’t fix the EHR systems. That’s why genetic testing is so rare. They profit from side effects. They profit from ER visits. They profit from chronic illness.
And now they’re telling YOU to carry a list? As if that’s the solution? No. No. No.
They’re gaslighting us. This is a trap. I’ve been researching this for 3 years. The truth is out there. You just have to look past the lies.
…I’m starting a support group. Join me. We’ll fight this.
athmaja biju
February 21, 2026 AT 15:35As an Indian man who has been on 11 medications since 2018, I can confirm: the system is broken. But this article is still too polite. We need to burn it down. Not just fix it.
Doctors in India don’t even check kidney function before prescribing statins. In the US, they check-but only if you ask. So who’s the real villain? The doctor? Or the system that lets them get away with it?
My mother died because they gave her the same dose as a 45-year-old man. She was 68. She weighed 48kg. She had diabetes. They didn’t adjust. They didn’t care.
This isn’t science. It’s negligence. And it’s genocide by prescription.