Every time you pick up a prescription, there’s a small piece of paper stuck to the bottle with writing that feels like it was meant for a doctor, not you. Lines like "take with food", "do not crush", or "refrigerate" seem simple-but they’re not. These are special instructions, and getting them wrong can mean your medicine doesn’t work, or worse, it hurts you.
According to a 2008 study, nearly half of all patients misunderstand these instructions. That’s not a small number-it’s millions of people taking pills at the wrong time, with the wrong food, or in the wrong way. And it’s not because they’re careless. It’s because the labels are confusing, scattered, and often written in a language most people don’t speak fluently.
What Are Special Instructions, Really?
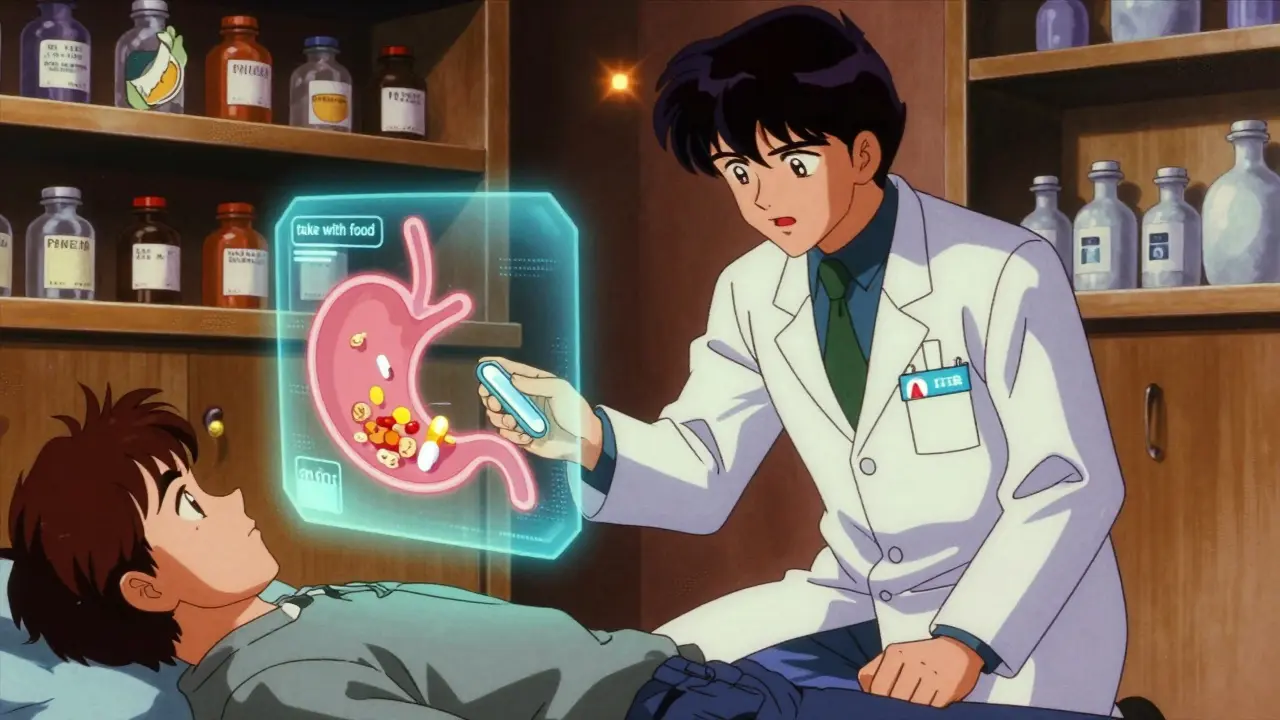
Special instructions aren’t just "take one pill daily." They’re the hidden rules that change how your medicine works. They tell you when to take it (on an empty stomach or after breakfast), how to store it (in the fridge or away from sunlight), and what to avoid (alcohol, certain foods, or other drugs). Some even say what not to do-like "do not crush" on a time-release tablet. Crush it, and you could get a dangerous overdose all at once.
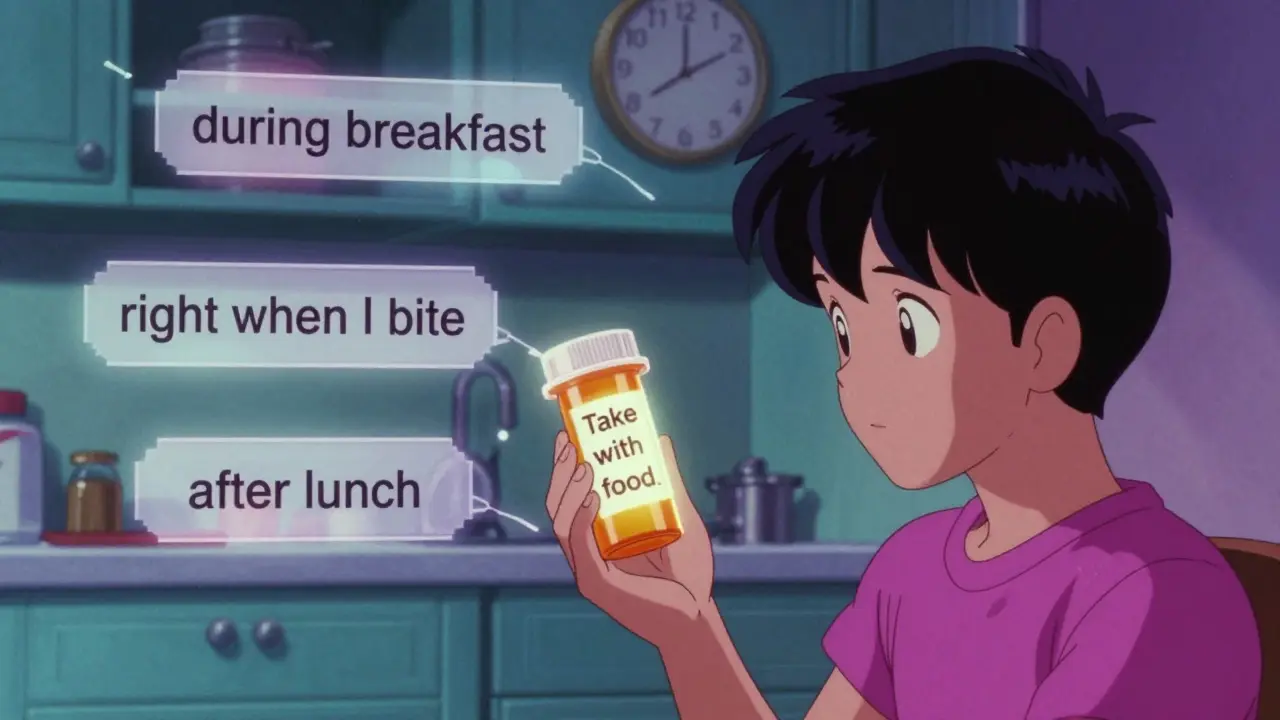
These instructions are legally required by the FDA. They’re not suggestions. In 2014, the FDA updated its rules to make sure these directions were clear enough to prevent mistakes. But clarity doesn’t always mean understanding. A 2021 Harvard study found that 41% of people think "take with food" means right when they start eating. Another 33% think it means during the meal. Only 26% know it means within 30 minutes of eating. That’s a huge gap.
Where Do You Even Find These Instructions?
They’re not always where you expect. In fact, they’re often hiding.
- 32% are printed directly on the bottle label
- 47% are on a small sticker stuck on the side
- 21% are in a separate paper insert you might toss without reading
That means you could have three different places to check. And if you miss one, you miss critical info. A 2022 Consumer Reports survey found that 54% of people had trouble finding these instructions at all. One in three admitted they’d missed something important-and didn’t even realize it.
Pharmacies don’t always place them the same way. Walgreens puts them on the bottle 87% of the time. CVS puts them in a separate sheet 63% of the time. If you switch pharmacies, you might be looking in the wrong spot.
Why Does This Even Matter?
Because mistakes cost lives-and money.
Medication errors tied to unclear labels cost the U.S. healthcare system $42 billion a year. That’s not just hospital bills. It’s emergency room visits, missed work, long-term damage, and even deaths. A 2019 Johns Hopkins study showed that when patients understood their special instructions correctly, medication errors dropped by 38%.
But here’s the catch: people with low health literacy-about 36% of U.S. adults-are more than twice as likely to mess up. They don’t know what "empty stomach" means. They think "every 12 hours" means 8 a.m. and 8 p.m., not 12 a.m. and 12 p.m. They don’t realize that "shake well" isn’t just a suggestion-it’s necessary to make sure the medicine is evenly mixed.
One of the most dangerous instructions? "Take on empty stomach." A patient forum with over 2 million users recorded 287 cases of people taking antibiotics or thyroid meds with breakfast, thinking it was fine. The result? The medicine didn’t absorb. The infection didn’t clear. The thyroid levels stayed off. And they went back to the doctor, confused and worse off.
Who’s Trying to Fix This?
The FDA isn’t ignoring the problem. In 2021, they launched the Enhanced Medication Labeling Initiative to make instructions clearer for high-risk drugs. They now require:
- Font size of at least 10 points
- High contrast between text and background
- Standardized phrases like "take on an empty stomach" instead of vague terms like "take before meals"
They’ve also started testing something new: augmented reality labels. Scan the bottle with your phone, and a short video plays showing how to take the medicine. It’s still a pilot, but early results are promising.
Pharmacists are on the front lines. A 2023 report found that 89% of positive pharmacy reviews mentioned pharmacists who took time to explain the instructions. That’s more than price, convenience, or speed. People value someone who slows down and makes sure they understand.
But not every pharmacy has the time. A University of Michigan study found that the average counseling session lasts just 2.1 minutes. Yet experts say you need at least 7.3 minutes to really understand your meds. That’s a big problem.
What You Can Do Right Now
You don’t have to wait for the system to fix itself. Here’s what actually works:
- Check all three places-the bottle, the sticker, and the paper insert. Don’t assume one is enough.
- Ask the pharmacist-not just "What’s this for?" but "What does ‘take with food’ mean here? Should I wait 30 minutes after eating?" Be specific.
- Write it down-if they say "take every 12 hours," write down the exact times: 7 a.m. and 7 p.m. Stick it on your fridge.
- Use a pill organizer-one with compartments for morning, afternoon, evening, and night. Mayo Clinic found these reduce timing errors by 47%.
- Request large-print labels-94% of U.S. pharmacies offer them for free. If you’re struggling to read, ask.
- Use a reminder app-apps like Medisafe or MyTherapy help track doses and send alerts. 62% of users say it improved their adherence.
If you’re not a native English speaker, you’re at higher risk. A 2022 UCSF study found Spanish-speaking patients misinterpreted "take with food" instructions 3.2 times more often than English speakers. Ask for translated materials. Most pharmacies have them.
The Bigger Picture
This isn’t just about reading labels. It’s about health literacy. About dignity. About being treated like someone who deserves to understand their own care.
Right now, 77 million U.S. adults have basic or below-basic health literacy. That’s nearly one in three. And the system still expects them to decode medical jargon on their own.
But change is coming. The FDA is proposing new rules by 2026 to standardize 12 key instructions across all prescriptions. Pharmacy chains are testing AI tools that adjust label language based on your reading level. And doctors can now bill for 5-minute counseling sessions specifically to explain these instructions.
Still, the biggest fix isn’t technology. It’s time. Time for pharmacists to slow down. Time for doctors to ask, "Do you understand?" instead of assuming they do. Time for patients to speak up and say, "I’m not sure what that means. Can you show me?"
Because your health shouldn’t depend on how well you can read tiny print on a sticker.
What If You Still Don’t Understand?
Don’t guess. Don’t assume. Don’t risk it.
Call your pharmacy. Ask for a pharmacist. Say: "I need help understanding the instructions on my prescription. Can we go over them together?"
If you’re on Medicare or Medicaid, you can request a free medication review. Many states offer this service. It’s not just a check-up-it’s a safety net.
And if you’ve ever taken a pill and thought, "Wait, is this right?"-you’re not alone. You’re not wrong to question it. You’re smart to ask.
What does "take with food" really mean on a prescription label?
"Take with food" means you should take your medication within 30 minutes of starting a meal. It does not mean "right when you bite into your food," nor does it mean "during the entire meal." The goal is to have food in your stomach to help your body absorb the drug properly and reduce nausea or stomach upset. Always confirm with your pharmacist what counts as "food"-a snack may not be enough.
Why are special instructions sometimes on a sticker and not the bottle?
Pharmacies often use stickers when the label space is limited, or when instructions change after the bottle is printed. This is common with new prescriptions, dosage adjustments, or when a drug has multiple possible instructions. Stickers are also used for high-risk medications that require extra warnings. Always check for stickers before taking any pill.
What should I do if I miss a dose because I didn’t understand the instructions?
Don’t double up. Call your pharmacist or doctor immediately. Taking two doses at once can be dangerous. For most medications, if you miss a dose by a few hours, take it as soon as you remember. If it’s almost time for the next dose, skip the missed one. But rules vary by drug-always check with a professional.
Can I crush a pill if it’s hard to swallow?
Only if the label says you can. Many pills-especially time-release, extended-release, or enteric-coated ones-are designed to release slowly. Crushing them can cause a dangerous overdose. If swallowing is hard, ask your pharmacist about liquid forms, dissolvable tablets, or alternative medications.
Are there tools to help me remember when to take my meds?
Yes. Pill organizers with morning, afternoon, evening, and night compartments reduce timing errors by nearly half. Medication reminder apps like Medisafe or MyTherapy send alerts and track your adherence. Many pharmacies also offer blister packs pre-filled with your daily doses. Ask your pharmacist about these options-they’re often free or low-cost.
What if I don’t speak English well? Can I get instructions in my language?
Yes. By law, most pharmacies must provide translated materials for common languages, including Spanish, Chinese, Vietnamese, and Arabic. You can also ask for a phone interpreter. Don’t rely on family members to translate medical instructions-misunderstandings can be dangerous. Always request official translated labels or a live translator from the pharmacy.
Why do some prescriptions have a Medication Guide?
The FDA requires a Medication Guide for about 250 high-risk prescription drugs-like blood thinners, antidepressants, and chemotherapy agents-where misunderstanding could lead to serious harm. These guides explain risks, side effects, and what to do in an emergency. They’re not optional. Always read them. If you didn’t get one, ask for it.
Is it safe to use leftover medication if the instructions say to throw it away after 14 days?
No. Medications that expire or degrade after a short time-especially liquids, eye drops, or insulin-can become ineffective or even toxic. The 14-day rule is based on how quickly the drug breaks down once opened. Even if it looks fine, it may not work. Always follow the discard date. Many pharmacies offer take-back programs for safe disposal.
Johanna Baxter
January 9, 2026 AT 23:50Why do pharmacies even bother with stickers? I once took my blood pressure med without reading the sticker and ended up in the ER because I didn’t know it had to be taken on an empty stomach. Now I treat every sticker like a bomb defusal manual. 🤯
Phil Kemling
January 11, 2026 AT 22:57It’s not just about clarity-it’s about power. The label is a tiny act of authority. The pharmacy prints it, the doctor prescribes it, the FDA mandates it-but the patient is left to decode it alone. Who gets to decide what’s ‘clear’? Not the person swallowing the pill.
Diana Stoyanova
January 12, 2026 AT 22:20Okay but let’s talk about how insane it is that we’re expected to be pharmacists now? 😤 I’m not a scientist, I’m a person trying to get through Monday. I don’t care if it’s ‘within 30 minutes of eating’-I just want to know if I can take it with my damn toast and coffee. And why is the answer always ‘it depends’? Like, can we PLEASE have a universal cheat sheet? I’d pay for an app that just says: ‘THIS MED = TAKE WITH BANANAS, NOT OATMEAL.’
Also, why do I have to ask for large print like I’m begging for mercy? It’s 2024. My phone can read signs on the street-why can’t my pill bottle?
And don’t get me started on the ‘Medication Guide’ they hand you like a pamphlet for a church bake sale. I’ve never read one. I don’t have time. I’m tired. I just want to live.
Pharmacists who take 7 minutes? I’d hug them. I’d send them flowers. I’d name my firstborn after them. Why is kindness the exception, not the rule?
And yes-I use Medisafe. It saved me. But why do I have to rely on an app to not die? This isn’t tech failure. It’s system failure.
Also, if you’re Spanish-speaking and they give you a translated label? That’s not a perk. That’s a human right. Period.
Stop treating health literacy like a bonus feature. It’s the foundation. We’re all just trying not to accidentally overdose on our own confusion.
Jenci Spradlin
January 14, 2026 AT 18:23lol i used to crush my migraine pills cause they were too big to swallow… until i got dizzy for 3 hours and called my doc. turns out they were time release. duh. now i use a pill cutter. cheap as hell. ask your pharmacist for one. they’ll give it to ya free. also, if you’re on medicaid, they’ll mail you a pill organizer. just ask. no one tells you this stuff.
Meghan Hammack
January 14, 2026 AT 23:21You’re not alone. I used to skip doses because I thought ‘take with food’ meant ‘if you feel like it.’ Then my thyroid went haywire. I cried in the pharmacy. The pharmacist didn’t judge. She sat down with me. Showed me the sticker. Wrote down the times. Gave me a free pill box. I still have it. I call her my angel. Don’t be shy. Ask. Say ‘I’m scared I’m doing this wrong.’ They’ve heard it a thousand times. They want to help. You deserve to feel safe with your meds.
Elisha Muwanga
January 16, 2026 AT 16:08This country is falling apart because people won’t take responsibility. If you can’t read a label, get glasses. If you can’t understand English, learn it. Don’t blame the system for your laziness. The FDA spent millions making these clearer. If you still don’t get it, maybe you shouldn’t be taking prescription drugs at all.
Maggie Noe
January 17, 2026 AT 16:04That 2.1 minute counseling stat broke me. 😔 I’ve been on 5 meds since last year. Only one pharmacist took the time. The rest just handed me the bottle like it was a fast food order. I’m not asking for a therapy session. I’m asking for 5 minutes of human connection. Can we make that a requirement? 🙏
Gregory Clayton
January 19, 2026 AT 11:57USA: where your life depends on whether you found a sticker on a bottle that a pharmacist slapped on while yelling into a headset. We spend billions on war but can’t print instructions big enough for seniors? This is why I hate this country sometimes.