Why Diets Fail and How Thinking Changes Everything
Most people who lose weight gain it back. Not because they lack willpower, but because they never changed how they think about food, hunger, and failure. A diet tells you what to eat. Behavioral weight loss therapy tells you why you eat the way you do-and how to stop the cycle before it starts.
It’s not about counting calories harder. It’s about catching the thought that says, "I’ve blown it, so I might as well finish the whole bag." That thought isn’t weakness. It’s a habit of the mind. And habits can be rewired.
What Is Cognitive Behavioral Therapy for Weight Loss?
Cognitive Behavioral Therapy, or CBT, was developed in the 1960s to treat depression and anxiety. By the 1980s, researchers at the University of Pennsylvania realized it could help people with obesity too. The idea? Your thoughts drive your behavior. If you believe "I can never eat what I want," you’ll rebel. If you think "One mistake means I’ve failed," you’ll quit.
CBT for weight loss isn’t just about eating less. It’s about changing the mental scripts that lead to overeating, emotional snacking, and giving up after a slip-up. Studies show people using CBT lose more weight than those on standard diets-8.2% on average versus 5.1% in six months. And they’re more likely to keep it off.
The Five Cognitive Strategies That Actually Work
Not all CBT is the same. The most effective programs use five core strategies, backed by clinical trials and real-world results.
- Cognitive Restructuring-This is where you challenge the lies your brain tells you. "I’ll never reach my goal." "I don’t deserve to eat healthy." These aren’t facts. They’re patterns. A therapist helps you replace them with realistic thoughts: "I’m learning. Progress isn’t perfect."
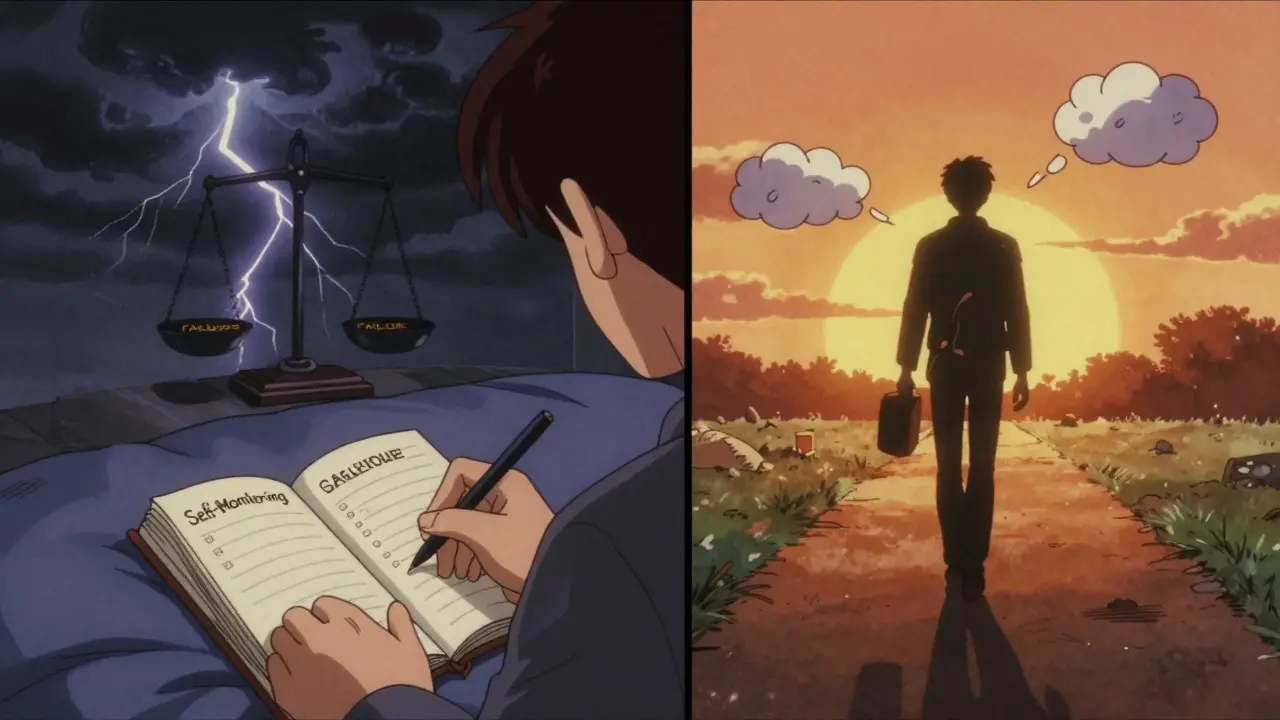
- Self-Monitoring-Writing down what you eat and how you feel isn’t about guilt. It’s about awareness. Studies show people who track their meals consistently lose 5-10% more weight. The key? Don’t judge. Just record. "I ate cake because I was stressed." That’s data, not failure.
- Stimulus Control-Your environment controls you more than you think. Keep junk food out of sight. Don’t eat in front of the TV. Use smaller plates. These aren’t tricks. They’re science. When triggers are removed, cravings lose power.
- Goal Setting-"Lose 50 pounds" is overwhelming. "Walk 20 minutes, three times this week" is doable. SMART goals-Specific, Measurable, Achievable, Relevant, Time-bound-work because they give your brain a clear path. Small wins build confidence.
- Relapse Prevention-You will slip. Everyone does. The question isn’t if, but how you respond. CBT teaches you to see a slip as feedback, not a disaster. A single cookie doesn’t erase a week of progress. It’s one data point. Adjust. Keep going.
Why CBT Beats Dieting Alone
Diets focus on food. CBT focuses on you.
One study compared people on a standard weight loss plan with those using CBT. The CBT group lost more weight, kept it off longer, and reported less depression and anxiety. Why? Because CBT doesn’t just change behavior-it changes your relationship with food.
Think about it: if you’re eating because you’re lonely, bored, or stressed, no diet will fix that. Only understanding the emotion behind the bite will.
CBT also works best for people with binge eating disorder. More than half of those treated no longer met the diagnosis five years later. That’s not just weight loss. That’s healing.
The Hidden Problem: Dropout Rates and Why CBT Keeps People in the Game
Most weight loss programs lose more than half their participants within six months. Standard diets? 54.4% drop out. CBT-based programs? Only 38.7%.
Why the difference? CBT doesn’t shame you. It doesn’t say "you failed." It says, "What happened? Let’s figure out what triggered it."
Therapists use Motivational Interviewing-a gentle, non-judgmental style-to help you find your own reasons to change. That’s powerful. People who feel in control stick with it longer. One study showed a 22% drop in dropout rates when CBT was paired with Motivational Interviewing.
Can You Do CBT on Your Own?
Yes-but with limits.
Apps like Noom and WeightWatchers Beyond the Scale use CBT principles. They’re better than nothing. But they’re not the same as working with a trained therapist. A 2023 review found app-based programs led to 3.2% average weight loss. Therapist-led CBT? 6.8%.
Why? Human connection matters. A therapist notices when you’re avoiding a topic. They catch your self-criticism before it becomes a habit. They adjust your plan when you’re stuck. That’s hard to replicate with an algorithm.
That said, internet-based CBT (ICBT) is getting better. A 2024 study showed structured online modules helped people lose weight and reduce stress. It’s not perfect, but for those without access to a therapist, it’s a real option.
Who Benefits Most From CBT?
CBT isn’t for everyone-but it’s especially powerful for certain groups:
- People with binge eating disorder
- Those who struggle with emotional eating
- People who’ve tried diets and kept regaining weight
- Anyone who feels guilty or ashamed about food
- Those with anxiety or depression tied to body image
If you’ve ever thought, "It’s not fair I have to work so hard," or "I’ll never be thin," CBT can help you let go of those thoughts. They’re not true. They’re just old habits.

The Reality Check: CBT Isn’t a Magic Bullet
Let’s be honest. CBT won’t make you lose 30 pounds in 3 months. The average weight loss is moderate-around 5-10% of body weight. And 30-35% of people regain some weight within a year.
But here’s the thing: CBT isn’t meant to be a quick fix. It’s a long-term skill set. Think of it like learning to drive. You don’t just memorize the rules. You practice. You make mistakes. You adjust. Eventually, it becomes automatic.
And when CBT is combined with medication-like GLP-1 agonists (semaglutide, tirzepatide)-results improve dramatically. The NIH is now funding major trials to see how CBT can help people stay on track after starting these drugs. Because even the best medicine won’t fix a mind stuck in old patterns.
Access and Cost: The Big Barrier
Here’s the hard truth: CBT is hard to find.
In the U.S., there’s only one certified CBT obesity specialist for every 125,000 people who could benefit. Insurance rarely covers more than 12 sessions. Many therapists don’t specialize in weight loss at all.
But things are changing. Group CBT programs are becoming more common-and just as effective as one-on-one therapy, but at one-third the cost. Some hospitals and clinics now offer them. Ask your doctor. Check with local mental health centers. Look for programs affiliated with universities.
If you’re in the UK, the NHS sometimes offers CBT for obesity through community health services. It’s not always easy to get, but it’s there.
What to Look For in a CBT Program
If you’re considering CBT for weight loss, here’s what to ask:
- Is the therapist trained specifically in CBT for obesity? (Not just general CBT)
- How many sessions are included? (Aim for 12-26)
- Do they use self-monitoring and goal setting?
- Do they address emotional eating and relapse prevention?
- Is there follow-up support after the program ends?
Good programs don’t just focus on the scale. They track mood, stress, confidence, and how you respond to setbacks. That’s the real measure of success.
Final Thought: It’s Not About Perfect. It’s About Persistent.
You don’t need to be perfect. You just need to keep showing up.
CBT teaches you that one bad meal doesn’t ruin your progress. One stressful day doesn’t erase your effort. It’s not about avoiding mistakes. It’s about learning how to bounce back.
The goal isn’t to never want cake. The goal is to want cake-and still choose what’s right for you. That’s real freedom. And that’s what CBT gives you.

Melissa Melville
February 1, 2026 AT 01:32Bryan Coleman
February 1, 2026 AT 08:56Naresh L
February 3, 2026 AT 07:35Sami Sahil
February 3, 2026 AT 16:38franklin hillary
February 3, 2026 AT 19:16Bob Cohen
February 5, 2026 AT 10:03Ishmael brown
February 6, 2026 AT 02:33Aditya Gupta
February 6, 2026 AT 07:14Nicki Aries
February 7, 2026 AT 14:09Nancy Nino
February 7, 2026 AT 15:13June Richards
February 9, 2026 AT 08:00