Antibiotic Selection Guide
Which Antibiotic Might Be Right for Your Situation?
This tool helps you understand which antibiotics are typically used for different infections. Note: This is for educational purposes only. Always consult your doctor for medical advice.
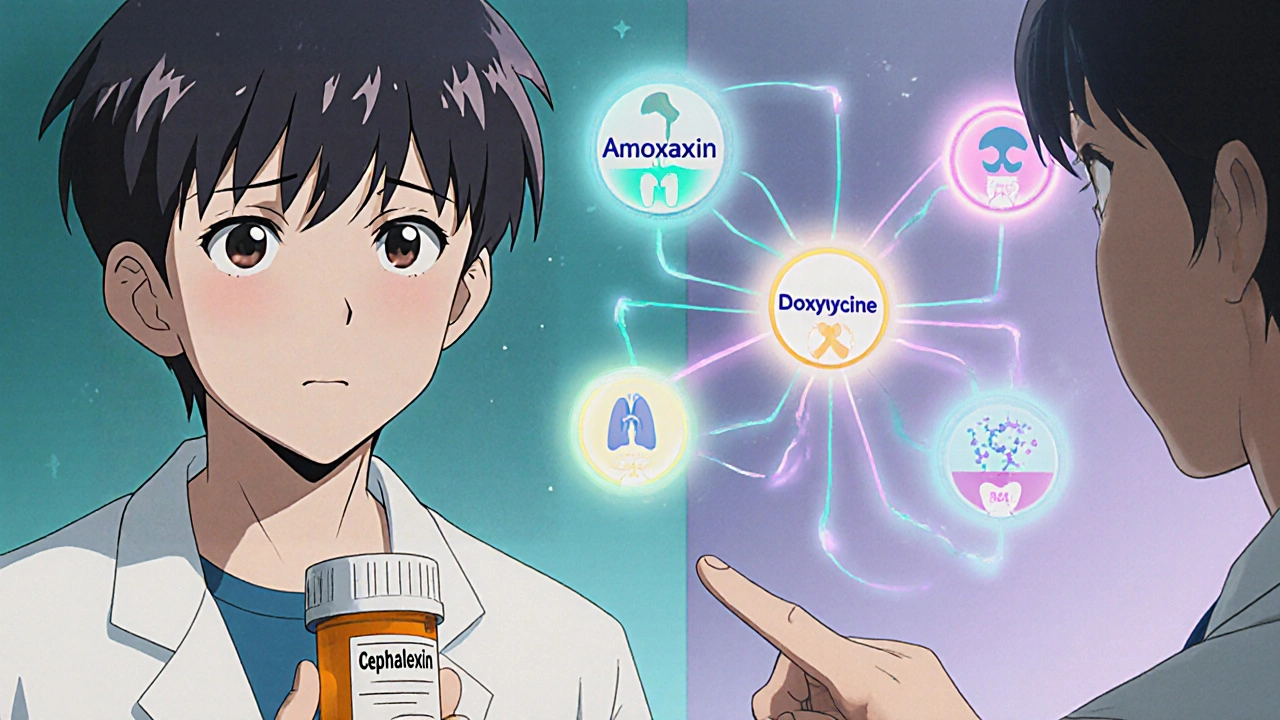
Antibiotics aren’t one-size-fits-all. If you’ve been prescribed cephalexin and are wondering if there’s a better option, you’re not alone. Many people ask: cephalexin works for me, but what if I’m allergic? What if it doesn’t clear up my infection? What else can I take? The truth is, several antibiotics can treat the same infections - but not all are equal. Choosing the right one depends on your infection type, medical history, allergies, and even your local bacteria patterns.
What is cephalexin, really?
Cephalexin is a first-generation cephalosporin antibiotic. It’s been around since the 1960s and is still widely used today. It’s sold under brand names like Keflex and is available as a generic, making it affordable. It works by breaking down the cell walls of bacteria, killing them or stopping them from multiplying.
Doctors commonly prescribe cephalexin for:
- Skin infections like cellulitis or impetigo
- Respiratory tract infections such as strep throat or mild pneumonia
- Urinary tract infections (UTIs)
- Bone and joint infections (like osteomyelitis)
It’s usually taken every 6 to 12 hours for 7 to 14 days. Most people tolerate it well, but side effects like nausea, diarrhea, or stomach upset are common. About 10% of people allergic to penicillin also react to cephalexin - so if you’ve had a penicillin rash or anaphylaxis, you need to be careful.
Why look at alternatives?
People switch from cephalexin for several real reasons:
- They had an allergic reaction
- It didn’t work after a few days
- They’re taking other meds that interact poorly
- They need something that works against different bacteria
- They’re pregnant, breastfeeding, or have kidney issues
Not all infections respond the same way. For example, cephalexin is weak against certain types of staph, like MRSA. It also doesn’t cover many anaerobic bacteria - the kind that cause abscesses or dental infections. That’s where other antibiotics come in.
Amoxicillin: The penicillin cousin
Amoxicillin is a penicillin-type antibiotic, often prescribed for ear infections, sinusitis, and strep throat. It’s similar to cephalexin in spectrum but has broader coverage against some Gram-negative bacteria like E. coli and H. influenzae.
Here’s how they compare:
| Feature | Cephalexin | Amoxicillin |
|---|---|---|
| Class | Cephalosporin | Penicillin |
| Best for | Skin, bone, urinary infections | Ear, sinus, respiratory infections |
| Penicillin allergy risk | ~10% cross-reactivity | High risk - avoid if allergic |
| Dosing frequency | 2-4 times daily | 2-3 times daily |
| Effectiveness against MRSA | No | No |
| Common side effects | Diarrhea, nausea | Diarrhea, rash, yeast infections |
If you’re not allergic to penicillin, amoxicillin is often just as effective - and sometimes more so - for respiratory infections. But if you’ve had a penicillin allergy, amoxicillin is off the table. Cephalexin might be your next option, unless you’re one of the 10% who react to both.
Doxycycline: The broad-spectrum option
Doxycycline is a tetracycline antibiotic. It’s not used for simple skin or bladder infections - it’s reserved for more complex cases. It’s great against bacteria that cephalexin can’t touch, like:
- Mycoplasma and chlamydia (common causes of pneumonia or STIs)
- Lyme disease
- Acne and rosacea (long-term low doses)
- Some tick-borne illnesses
It’s taken once or twice daily and works well for infections in the lungs, sinuses, or even tick bites. But it has downsides:
- Must be taken on an empty stomach - food and dairy reduce absorption
- Can cause severe sunburn - avoid direct sunlight
- Not safe for kids under 8 or pregnant women - it stains developing teeth
Compared to cephalexin, doxycycline is a bigger gun. It’s not a first-line replacement unless your infection involves unusual bacteria. If your doctor suspects Lyme or a resistant skin infection, they might jump straight to doxycycline instead of trying cephalexin first.

Clindamycin: For resistant or deep infections
Clindamycin is a go-to when cephalexin fails - especially for skin abscesses, dental infections, or suspected MRSA. It’s one of the few oral antibiotics that works well against anaerobic bacteria and many strains of staph that resist penicillin and cephalosporins.
It’s often used when:
- A skin infection is getting worse despite cephalexin
- There’s a dental abscess with swelling
- A patient is allergic to penicillin and cephalosporins
But clindamycin has a big red flag: it can cause a dangerous gut infection called C. difficile colitis. This can happen even weeks after finishing the course. Symptoms include severe diarrhea, cramping, and fever. It’s rare, but serious - so doctors avoid it unless necessary.
Compared to cephalexin, clindamycin is stronger but riskier. It’s not something you take for a simple UTI. It’s a backup plan for tough, stubborn, or deep infections.
Other alternatives you might hear about
There are other antibiotics sometimes discussed as alternatives:
- Trimethoprim-sulfamethoxazole (Bactrim): Good for UTIs and some skin infections. Not great for respiratory bugs. Can cause serious rashes in some people.
- Fluoroquinolones (ciprofloxacin, levofloxacin): Powerful but restricted now due to serious side effects like tendon rupture and nerve damage. Only used for severe infections like complicated UTIs or kidney infections.
- Azithromycin: A macrolide. Used for respiratory infections and STIs. Less effective for skin or bone infections than cephalexin.
These aren’t direct swaps for cephalexin. Each has its own niche. You don’t trade cephalexin for ciprofloxacin just because it sounds stronger - you do it because your infection requires it.
How your doctor picks the right one
There’s no single "best" antibiotic. The decision is based on:
- Where the infection is: Skin? Lungs? Bladder? Each location has common bacteria.
- How bad it is: Mild cellulitis? Maybe cephalexin. Deep abscess? Clindamycin or surgery.
- Your history: Allergies, kidney function, past antibiotic use, pregnancy.
- Local resistance: In some areas, MRSA is common in skin infections - cephalexin won’t cut it.
- Cost and access: Generic cephalexin costs under $10 in the U.S. Doxycycline is cheap too. Newer antibiotics can cost hundreds.
Doctors often start with cephalexin because it’s safe, cheap, and works for most common infections. If it doesn’t work after 48-72 hours, they switch. That’s not failure - it’s standard practice.
What you should do if cephalexin isn’t working
If you’ve been on cephalexin for 2-3 days and feel worse - or your fever, swelling, or pain is getting worse - don’t wait. Call your doctor. Don’t double the dose. Don’t take leftover antibiotics. Don’t assume it’s "just getting worse before it gets better."
Signs you need help now:
- Fever above 38.5°C (101.3°F) that won’t go down
- Red streaks spreading from the infection site
- Difficulty breathing or swallowing
- Severe diarrhea (could be C. diff)
Your doctor might order a culture - swabbing the infection to see exactly what bacteria are there. That’s the only way to know for sure which antibiotic will work. Guessing can delay recovery.
When to avoid alternatives
Some people try to self-switch antibiotics because they’re afraid of side effects or think one is "stronger." That’s dangerous.
- Don’t take doxycycline if you’re pregnant - it harms the baby’s teeth and bones.
- Don’t use clindamycin for a simple UTI - you’re risking C. diff for no reason.
- Don’t use azithromycin for a skin infection - it’s not effective against the usual bugs.
Each antibiotic has a job. Using the wrong one doesn’t just waste time - it can make the infection worse, or lead to antibiotic resistance.
Bottom line: Cephalexin is a solid first choice - but not always the right one
Cephalexin is a reliable, affordable, and effective antibiotic for many common infections. But it’s not magic. If you’re not improving, or you have allergies, or your infection is deep or unusual, other options exist - and they’re often better.
The key is not to pick the "best" antibiotic - it’s to pick the right one for your situation. That’s why you need a doctor’s judgment, not a Google search.
If you’ve had a bad reaction to cephalexin, keep a list of what didn’t work. That helps your doctor choose the next option faster. If you’re unsure why you were given a certain antibiotic, ask. Understanding your treatment helps you stick with it - and know when to call back.
Can I take amoxicillin instead of cephalexin if I’m allergic to penicillin?
No. If you have a confirmed penicillin allergy - especially one that caused hives, swelling, or trouble breathing - you should avoid amoxicillin and other penicillins. About 10% of people allergic to penicillin also react to cephalexin, so you may need a non-beta-lactam antibiotic like doxycycline or clindamycin instead. Always check with your doctor before switching.
Is clindamycin stronger than cephalexin?
It’s not about strength - it’s about coverage. Clindamycin works against bacteria that cephalexin can’t, like MRSA and anaerobic bacteria. That makes it more effective for deep skin infections, abscesses, or dental infections. But it carries a higher risk of causing C. difficile diarrhea. Cephalexin is safer for simple infections. Use clindamycin only when needed.
Why did my doctor switch me from cephalexin to doxycycline?
Doxycycline is often chosen when the infection might be caused by atypical bacteria - like those causing pneumonia, Lyme disease, or acne-related infections. If your symptoms didn’t improve with cephalexin, or if you have signs of a tick bite, acne flare, or respiratory illness with no clear source, doxycycline covers a wider range of bacteria. It’s not a random switch - it’s based on likely causes.
Can I take cephalexin if I’m pregnant?
Yes. Cephalexin is classified as Category B by the FDA, meaning it’s considered safe during pregnancy. It’s often used to treat UTIs and skin infections in pregnant women. However, always inform your doctor you’re pregnant before starting any antibiotic. They’ll choose the safest option for you and your baby.
What should I do if cephalexin gives me diarrhea?
Mild diarrhea is common with cephalexin and often goes away after finishing the course. Drink plenty of fluids and avoid dairy or spicy foods. If diarrhea becomes severe, watery, bloody, or lasts more than 2 days after stopping the antibiotic, contact your doctor immediately. It could be C. difficile, which needs specific treatment.
Are there natural alternatives to cephalexin?
No. While some natural products like honey, garlic, or tea tree oil have mild antibacterial properties, none can reliably treat bacterial infections like cellulitis, pneumonia, or UTIs. Relying on them instead of antibiotics can lead to serious complications, including sepsis. Antibiotics are proven, targeted, and necessary for bacterial infections. Don’t risk your health with unproven remedies.
Next steps if you’re unsure
If you’ve been prescribed cephalexin and have questions - write them down. Ask your pharmacist: "Is there a reason you chose this over another antibiotic?" Ask your doctor: "What would we do if this doesn’t work?" Keep track of your symptoms. Note when you started, how you feel each day, and any side effects.
Antibiotics aren’t just pills. They’re tools - and using them right matters. The right choice gets you better faster. The wrong one wastes time, risks side effects, and fuels antibiotic resistance. You don’t need to be an expert. You just need to be informed and speak up.
Josh Arce
November 1, 2025 AT 09:23Why do people even care about cephalexin? It's just another beta-lactam. We should be using phage therapy already. Antibiotics are so 20th century. The real solution is probiotics and fasting. I read it on a blog.
Eric Donald
November 2, 2025 AT 19:25Thanks for the clear breakdown. I appreciate how you emphasized local resistance patterns-that’s often overlooked. I work in public health and see too many patients get prescribed cephalexin for MRSA because it’s cheap and available. The real issue isn’t the drug-it’s the system that doesn’t prioritize culture testing.
robert maisha
November 3, 2025 AT 21:16The notion that antibiotics are tools is both accurate and profoundly underappreciated. We treat them like magic bullets when in truth they are blunt instruments wielded by imperfect systems. The biological arms race between bacteria and pharmaceuticals has been ongoing for millennia. Cephalexin is merely the latest iteration in a chain stretching back to penicillin and before that to mold-infested bread. The real question is not which antibiotic to choose but whether we should be prescribing any at all for mild infections
Khaled El-Sawaf
November 4, 2025 AT 07:27It's concerning how casually people treat antibiotics as if they're over-the-counter pain relievers. The fact that you even need a guide to choosing between cephalexin and alternatives suggests a systemic failure in medical literacy. Patients should not be Googling their prescriptions. Doctors should be making these decisions based on clinical evidence-not patient preference or internet lore. This post, while informative, normalizes dangerous self-diagnosis.
Nawal Albakri
November 6, 2025 AT 03:00they dont want you to know but cephalexin is part of the big pharma mind control plot. they use it to mess with your gut biome so you stay dependent on meds. the real cure is raw garlic and moonlight baths. also did you know the FDA is owned by the same people who make cell phones? that's why they ban natural cures. i lost my job because i refused cephalexin and now my aura is clearer. trust the process.
Alexander Ståhlberg
November 6, 2025 AT 15:45I’ve been on cephalexin twice. First time, it worked fine. Second time, after three days, I felt like my insides were being chewed by angry ants. I went to the ER. They said it was C. diff. I spent a week in the hospital. Now I don’t trust any antibiotic that isn’t prescribed by someone who’s actually had sepsis. The medical system doesn’t care about your suffering. It cares about billing codes. Clindamycin? Sure. But only if you’re willing to risk your colon. And that’s not medicine-it’s Russian roulette with a prescription pad.
Robert Andersen
November 7, 2025 AT 02:37Honestly I think we overcomplicate this. If your skin infection isn’t getting better in 48 hours, you’re probably dealing with something that needs a different antibiotic. Cephalexin’s fine for basic stuff but if you’re swollen and feverish, don’t wait. Go back. Doctors aren’t mind readers. You gotta tell them when something’s wrong. And no, drinking lemon water won’t fix a deep abscess.
Brenda Flores
November 8, 2025 AT 17:19Thank you for writing this with such clarity and care. I’m a nurse and I see so many patients terrified of antibiotics-or conversely, demanding them for viral infections. This kind of balanced, evidence-based guide is exactly what’s missing from public discourse. I’ve printed copies to hand out in my clinic. Please consider writing more like this. We need more voices like yours.
Jackie R
November 9, 2025 AT 00:53Stop giving people choices. Cephalexin is the standard. If it doesn’t work, it’s not the drug-it’s the patient. Stop blaming the medicine. Stop Googling. Just take the pill. America is falling apart because everyone thinks they’re a doctor.
Megan Oftedal
November 10, 2025 AT 09:25Hey, I just wanted to say I love how you included the pregnancy info! I’m 28 weeks and was freaking out about my UTI. Cephalexin was my only safe option and I didn’t even know that. Thank you for being so thorough. Also, your table? Chef’s kiss. I shared this with my mom and she cried. Not because she’s emotional (she’s not) but because she finally understood why the doctor picked it. You made a difference.
Musa Aminu
November 10, 2025 AT 13:42Y’all in the US always think your antibiotics are the best. In Nigeria, we’ve been treating cellulitis with local herbs for centuries. Cephalexin? It’s just a Western placebo. We don’t need your pills. We have neem, bitter leaf, and ancestral wisdom. Your overprescribing is why the world is full of superbugs. You think you’re smart? You’re just lazy. We don’t need your science-we need your respect.