Psoriasis isn’t just a skin condition-it’s your immune system going rogue. Instead of protecting you, it attacks your own skin, forcing skin cells to multiply too fast and pile up into thick, red, flaky patches. This isn’t caused by dirt or poor hygiene. It’s an autoimmune response, and while you can’t cure it, you can stop a lot of the flares by understanding what sets them off. Three big triggers stand out: stress, infection, and skin barrier damage. Get these under control, and you take back power over your symptoms.
Stress Doesn’t Just Feel Bad-It Flares Your Psoriasis
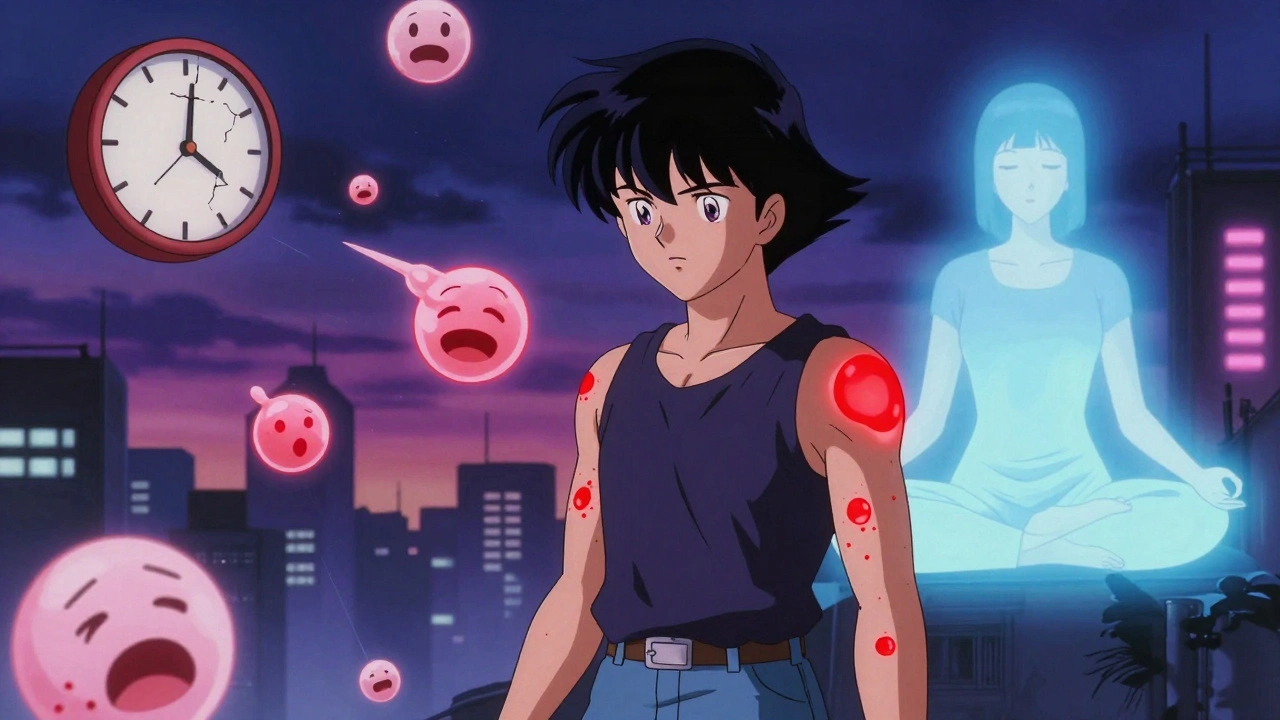
You know stress when you feel it: racing heart, tense shoulders, sleepless nights. But what you might not realize is that your body’s stress response is directly fueling your psoriasis. When you’re under pressure, your brain signals your adrenal glands to pump out cortisol and other stress hormones. These don’t just make you feel anxious-they trigger inflammation. And in psoriasis, inflammation is the engine that drives flares.
Studies show that nearly 70% of people with psoriasis say stress makes their symptoms worse. Even positive stress-like a promotion, a wedding, or moving-can set off a flare. One patient on Reddit shared that after his mother passed away, his mild psoriasis exploded within three months, covering 30% of his body. That’s not coincidence. Stress activates immune cells called T-cells and releases cytokines like IL-17 and IL-23, the exact same chemicals targeted by expensive biologic drugs.
And here’s the cruel twist: psoriasis causes stress, and stress makes psoriasis worse. It becomes a loop. You see a new patch, you panic, you sleep less, you feel more anxious, and then-boom-another flare. Breaking that cycle isn’t about being ‘positive.’ It’s about managing your biology. Daily mindfulness meditation for just 20 minutes has been shown to lower cortisol by 25% in eight weeks. Regular exercise, therapy, or even journaling can cut flare frequency by 30% or more. You don’t need to eliminate stress-you just need to stop letting it control your immune system.
Infections Are Silent Flare Triggers-Especially Throat Infections
Think of your immune system like a security guard. Sometimes, it gets confused. When a virus or bacteria invades, it doesn’t just fight the invader-it accidentally turns on your skin cells too. That’s what happens in psoriasis.
Strep throat is one of the most documented triggers, especially in kids and young adults. A strep infection can cause guttate psoriasis-small, drop-like spots that appear suddenly all over the body. It’s not the bacteria itself that damages the skin. It’s the immune system’s overreaction. The body releases proteins called antimicrobial peptides and activates a pathway involving RIG-I and IL-23, which then tells skin cells to multiply like crazy.
But it’s not just strep. Colds, flu, sinus infections, and even COVID-19 have been linked to psoriasis flares. People with HIV, despite having weakened immune systems, often see their psoriasis worsen-a paradox that shows how complex this disease is. The key takeaway? Don’t ignore infections. Get your flu shot. Wash your hands. Treat a sore throat early. One study found that getting the seasonal flu vaccine reduced infection-triggered flares by 35% in psoriasis patients.
If you notice a sudden outbreak of small red spots after a cold or sore throat, don’t assume it’s just a rash. It could be guttate psoriasis. See a dermatologist. Early treatment can stop it from turning into long-term plaque psoriasis.

Your Skin Barrier Isn’t Just a Cover-It’s a Shield
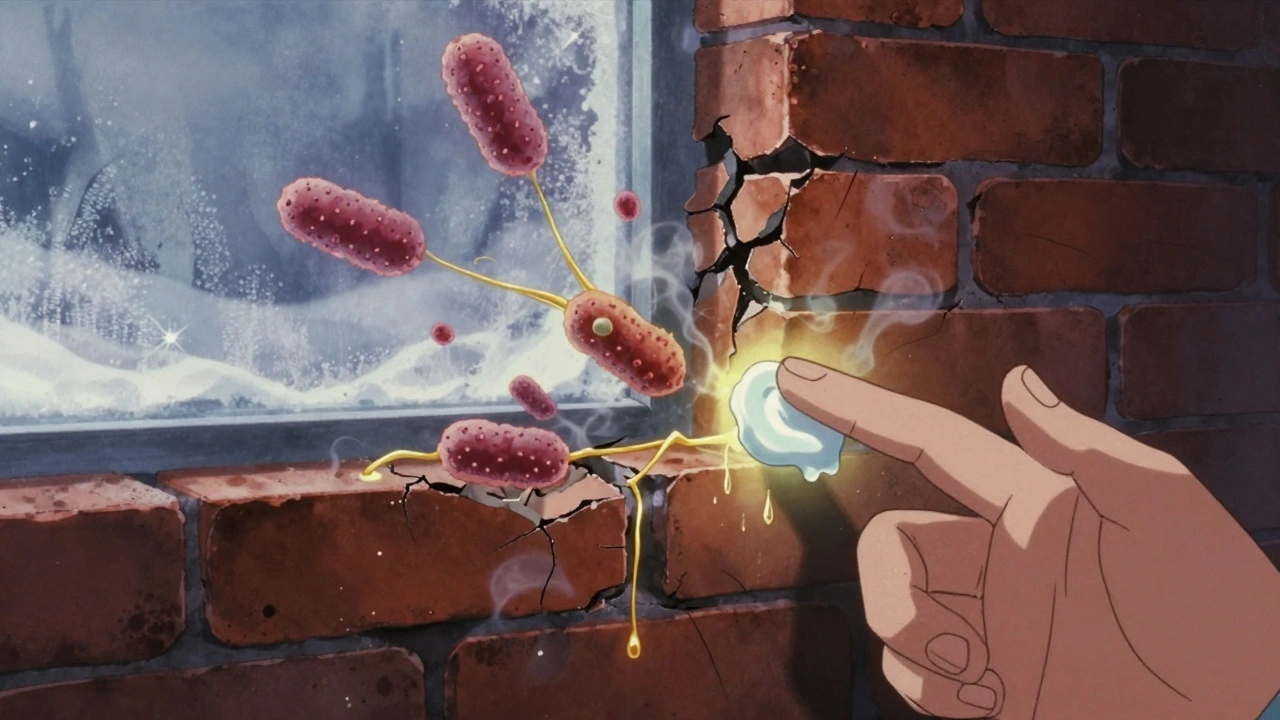
Think of your skin like a brick wall. The bricks are skin cells, and the mortar is natural oils and proteins that hold them together. In psoriasis, that wall is cracked. The LCE gene family, which helps build this barrier, is often faulty in people with psoriasis. When the barrier breaks down, moisture escapes, irritants get in, and bacteria start to grow where they shouldn’t.
This isn’t just dry skin. It’s a trigger. Research shows that when the skin barrier is damaged, bacteria like Staphylococcus aureus multiply and release toxins that activate immune cells in the skin. These cells then release IL-17 and IL-22, the same inflammatory signals that cause plaques. In mouse studies, applying topical antibiotics to damaged skin reduced psoriasis-like lesions by cutting down on these inflammatory chemicals.
And it’s not just about what you do to your skin-it’s about what you avoid. Harsh soaps with a high pH (above 5.5) strip away natural oils. Hot showers dry you out. Fragrances and alcohol in lotions irritate the barrier. Even minor injuries-bug bites, sunburns, scratches, or even tight clothing-can trigger the Koebner phenomenon, where psoriasis forms exactly where the skin was injured. One dermatology practice found that 45% of new plaques started at sites of unnoticed insect bites or tiny abrasions.
Fixing your barrier isn’t complicated. Use fragrance-free moisturizers with ceramides twice a day-morning and night. Keep your indoor humidity between 40% and 60%. Take lukewarm showers, not hot. Pat your skin dry, don’t rub. And if you’re going outside in winter, cover up. Cold, dry air is a trigger for 68% of psoriasis patients.
What You Can Do Right Now
Knowing your triggers is half the battle. The other half is acting on them. Here’s what works, based on real patient data and clinical guidelines:
- Track your flares. Keep a simple journal: note when flares happen, what you were doing, how stressed you felt, if you were sick, and what products you used. After a few months, patterns emerge. You’ll start to see, ‘Every time I get a cold, I flare.’ Or, ‘I break out after skipping moisturizer for two days.’
- Moisturize like it’s your job. Use ceramide-based creams or ointments (not lotions) every morning and night. Apply right after showering while skin is still damp. Ointments like petroleum jelly are cheaper and just as effective.
- Protect your skin. Wear gloves in cold weather. Use insect repellent. Avoid scratching. If you itch, put on a cool, damp cloth instead. Treat cuts and scrapes immediately with an antibiotic ointment and a bandage.
- Manage stress daily. Try 10 minutes of breathing exercises. Walk outside. Listen to music. Therapy isn’t a luxury-it’s part of your treatment plan. Studies show patients who do mindfulness or CBT reduce flare frequency by 30-50%.
- Stay up to date on vaccines. Get your flu shot every year. Ask your doctor about pneumococcal and COVID boosters. Preventing infections prevents flares.
What Doesn’t Work
There’s a lot of noise out there. You’ll hear that gluten-free diets cure psoriasis, or that turmeric is a miracle cure. Some people swear by them. But the science doesn’t back most of it. A 2022 survey of over 1,200 psoriasis patients found that while 32% reported dairy made their symptoms worse, and 25% said gluten did, only a small fraction saw real improvement on elimination diets. That doesn’t mean it doesn’t help some people-but it’s not a universal fix.
Same with ‘natural’ remedies. Aloe vera might soothe a red patch, but it won’t stop the immune system from attacking. Avoid harsh scrubs, lemon juice, or apple cider vinegar on plaques-they can burn and trigger more flares.
And don’t wait until you’re covered in plaques to act. Prevention beats treatment every time. The goal isn’t to be perfect. It’s to reduce flare frequency and severity. Even cutting flares in half can mean the difference between hiding your skin and living freely.
The Future Is Personalized
Doctors are starting to use AI and wearable tech to predict flares before they happen. Imagine a smartwatch that tracks your heart rate variability, sleep, and stress levels-and sends you a notification: ‘High stress detected. Apply moisturizer and take 10 minutes to breathe.’ That’s not science fiction. It’s coming within the next five years.
Meanwhile, new biologics are targeting the exact pathways triggered by stress and infection. One recent drug targeting IL-23 helped 89% of patients achieve 90% skin clearance in just 16 weeks. But even the best drug won’t work if you’re constantly stressed, sick, or scrubbing your skin raw.
Psoriasis is complex. But it’s not random. Your flares aren’t happening by chance. They’re signals. Listen to them. Manage your stress. Treat infections early. Protect your skin. You’re not just treating a rash-you’re calming your immune system.
Can stress cause psoriasis for the first time?
Yes. While psoriasis is genetic, stress can be the trigger that turns on the disease in someone who carries the genes. Many people report their first major flare happening within a year of a major life event like a breakup, job loss, or death in the family. Stress doesn’t cause psoriasis by itself, but it can be the spark that starts it.
Is psoriasis contagious?
No. Psoriasis is an autoimmune condition, not an infection. You can’t catch it from touching someone’s skin, sharing towels, or being near them. The plaques look scary, but they’re not infectious. The real risk is misunderstanding the condition-people with psoriasis often face stigma because others think it’s contagious or caused by poor hygiene.
Can cold weather make psoriasis worse?
Yes. Cold, dry air strips moisture from the skin and weakens the skin barrier. About 68% of psoriasis patients say their symptoms get worse in winter. Using a humidifier at home, wearing protective clothing, and moisturizing more often can help. Sunlight often helps psoriasis-but only in moderation. Too much sun can burn the skin and trigger flares in some people.
What’s the best moisturizer for psoriasis?
Look for thick creams or ointments with ceramides, hyaluronic acid, or petrolatum. Avoid anything with fragrance, alcohol, or dyes. Brands like CeraVe, Cetaphil, and Eucerin have psoriasis-friendly lines. Ointments (like plain petroleum jelly) work better than lotions because they seal in moisture longer. Apply right after bathing while your skin is still damp.
Should I avoid all infections if I have psoriasis?
You can’t avoid all infections, but you can reduce your risk. Wash your hands often, get vaccinated (flu, pneumonia, COVID), and treat sore throats or sinus infections early. If you notice a sudden outbreak of small red spots after a cold, see a dermatologist-it could be guttate psoriasis, which responds well to early treatment.
Does losing weight help psoriasis?
Yes. Fat tissue produces inflammatory chemicals, and people with obesity are more likely to have severe psoriasis. Losing even 5-10% of body weight can improve symptoms significantly. Exercise also helps reduce stress and improve skin barrier function. It’s not a cure, but it’s one of the most effective lifestyle changes you can make.
Paul Dixon
December 11, 2025 AT 05:24Man, I never realized stress could do that to my skin. I thought psoriasis was just "bad luck" until I started tracking my flares after my divorce. Turns out, every time I skipped meditation, boom - new patches. Now I do 10 minutes of breathing before bed. Not magic, but it helps.
Also, moisturizing after showers? Game changer. I used to skip it. Now I treat it like brushing my teeth.
Jimmy Kärnfeldt
December 12, 2025 AT 17:36It’s wild how your body holds onto trauma like that. Psoriasis isn’t just skin-deep - it’s emotional debris crystallizing on your epidermis. The immune system doesn’t care if you’re "strong" or "positive." It just reacts. And honestly? The fact that mindfulness lowers cortisol by 25% in 8 weeks? That’s not woo-woo. That’s biology whispering back.
We treat skin like a surface problem. But it’s a mirror. And we keep ignoring what it’s trying to say.
Ariel Nichole
December 13, 2025 AT 23:29I’ve had psoriasis for 12 years and this is the most practical post I’ve ever read. No fluff. Just facts. I’m gonna start tracking my flares like they said - maybe I’ll finally figure out why I flare every time I eat out. Probably the soap at the restaurant sink…
matthew dendle
December 15, 2025 AT 12:59lol so if i stop being stressed and wash my hands i cure psoriasis? wow. why didnt anyone think of that before the 200k dollar biologics? also aloe vera burns? no shit sherlock. next u gonna tell me water is wet
Mia Kingsley
December 15, 2025 AT 14:29Ugh this is so basic. Everyone knows stress causes flares. But what about the real cause? EMFs. 5G. Glyphosate. The government doesn't want you to know. I went gluten-free and got 80% better but no one listens. Also I only use coconut oil and moonwater. The dermatologist is just part of the pharma cartel.
Jean Claude de La Ronde
December 16, 2025 AT 05:57So you're telling me the same cytokines targeted by $10k/month drugs are also activated by crying over your dead mom? That’s poetic. And horrifying. We’ve turned human suffering into a biochemical equation. And then sold us creams to fix it.
Meanwhile, my cousin in Quebec just slapped on some birch sap and called it a day. He’s fine. Coincidence? Maybe. Or maybe we’re overcomplicating what’s simple.
Monica Evan
December 16, 2025 AT 23:53Y’all need to stop treating psoriasis like a villain to defeat. It’s more like a misfired alarm system. You don’t disable the alarm - you recalibrate it.
Also - if you’re using scented lotion on plaques, stop. It’s like pouring vinegar on a cut. I used to do it because I thought "it smells nice." Now I use plain CeraVe and feel like I’ve been given a gift. No hype. Just ceramides.
And yes - cold weather is the worst. I keep a humidifier running 24/7 in winter. My skin doesn’t crack anymore. Small wins, folks.
Aidan Stacey
December 18, 2025 AT 04:37THIS. THIS IS THE POST I’VE BEEN WAITING FOR MY WHOLE LIFE. I’ve been hiding in hoodies for 15 years. I thought I was broken. Turns out I just needed to know: stress = fuel. Infection = spark. Dry skin = open door.
I started moisturizing. I got the flu shot. I took a walk every day. Three months later? My arms are almost clear. I cried in the shower. Not from sadness. From relief.
You’re not alone. And it’s not your fault. Your body’s just yelling. Now you know how to listen.
Katherine Liu-Bevan
December 19, 2025 AT 11:30The Koebner phenomenon is underdiscussed. I developed a plaque on my wrist from a tiny scratch I didn’t even notice. It took months to realize the connection. Now I treat every minor injury like a potential trigger - clean it, cover it, moisturize around it. Simple, but effective.
Also, avoid wool. It’s not just itchy - it’s inflammatory. Cotton or bamboo fabrics are non-negotiable for me. And yes, humidity matters. I moved from Arizona to Seattle and my skin improved overnight.
Lisa Stringfellow
December 20, 2025 AT 05:37Wow. So after all this, the solution is... moisturizer and deep breathing? No wonder people think psoriasis is "just in your head." If this was a drug, it’d be off the market for being too basic. And don’t even get me started on the "AI watch" prediction nonsense. You’re telling me my watch will tell me to breathe... instead of just letting me live my life?