A cerebral aneurysm isn’t something you hear about until it’s too late. For most people, it’s silent-until it isn’t. About cerebral aneurysm affects 1 in 30 adults, but only a fraction ever rupture. The real question isn’t whether you have one-it’s whether it will burst, and what you can do about it.
What Exactly Is a Cerebral Aneurysm?
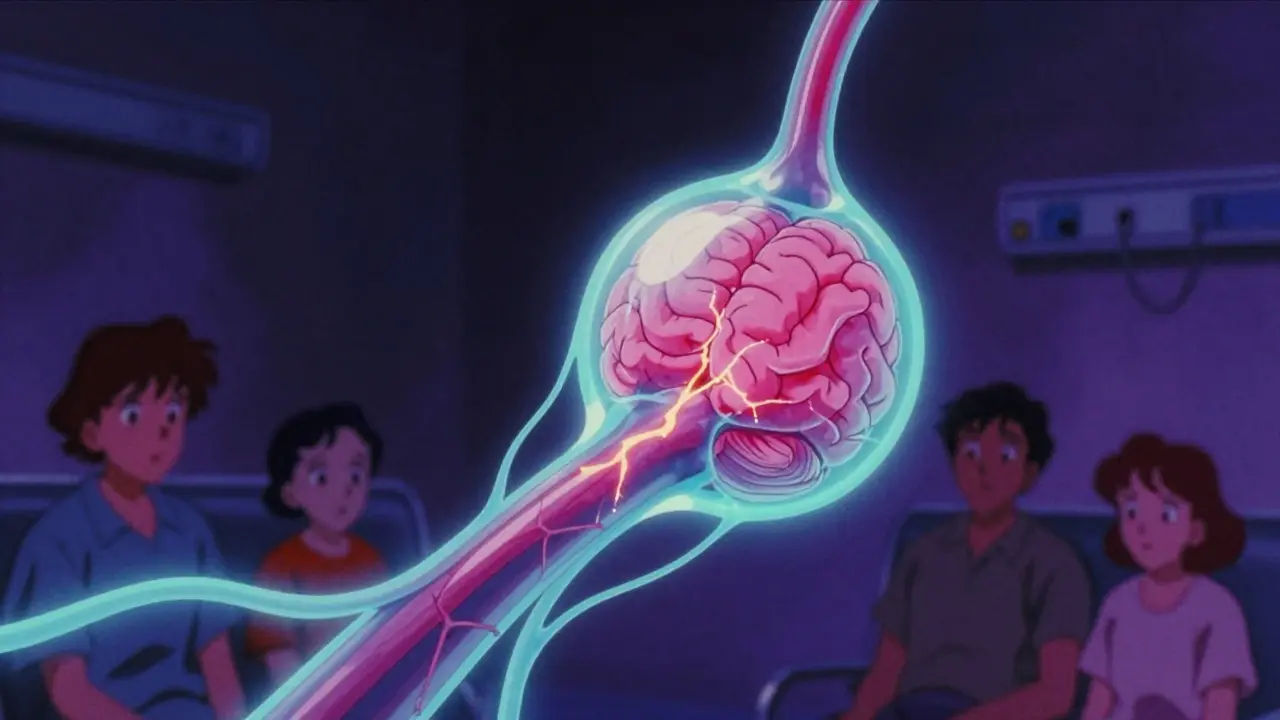
A cerebral aneurysm is a weak spot in the wall of a brain artery that balloons out like a tiny blister. It’s not a tumor. It’s not a clot. It’s a structural failure in the vessel itself. Think of it like a bulge in an old garden hose under constant pressure. Most stay small and never cause trouble. But when that bulge bursts, blood floods into the space around the brain-a subarachnoid hemorrhage. That’s a medical emergency. Around 30 to 40% of people die within the first day. Many others are left with permanent brain damage.
These aneurysms form over years, often without symptoms. They’re usually found by accident during scans for headaches, dizziness, or other unrelated issues. The good news? Most never rupture. The bad news? You can’t predict which ones will.
Who’s Most at Risk for Rupture?
Not everyone with an aneurysm is equally likely to bleed. Risk isn’t random. It’s shaped by biology, behavior, and location.
- Age matters. If you’re over 65, your rupture risk is nearly three times higher than someone in their 40s.
- Gender plays a role. Women are 1.6 times more likely than men to develop aneurysms-and more likely to have them rupture.
- Family history is a red flag. If two or more close relatives had one, your risk jumps fourfold.
Then there are the habits you can change:
- High blood pressure. Systolic pressure above 140 mmHg triples your rupture risk.
- Smoking. Current smokers have more than three times the risk of non-smokers. The more you smoke, the worse it gets-10+ cigarettes a day raises risk by 47%.
- Alcohol. More than 14 drinks a week increases rupture chances by 32%.
These aren’t just statistics. They’re actionable. Quitting smoking cuts rupture risk by over half within two years. Controlling blood pressure isn’t optional-it’s life-saving.
Size, Shape, and Location: The Trifecta of Danger
Not all aneurysms are created equal. Three features tell doctors how dangerous yours might be:
- Size. An aneurysm larger than 7 mm has a 3.1 times higher risk of rupture than smaller ones. But here’s the catch: some small ones rupture anyway.
- Shape. A round aneurysm is less risky. If it has bumps, lobes, or daughter sacs, your risk jumps nearly threefold.
- Location. Some spots in the brain are ticking time bombs. Aneurysms at the anterior communicating artery (AComm) are especially dangerous-they rupture even when they’re under 5 mm. Middle cerebral artery aneurysms also carry high risk, with rupture rates nearly four times higher than average.
That’s why location matters more than size sometimes. A 4 mm aneurysm in the AComm can be riskier than a 9 mm one in a safer spot. This is why doctors don’t just look at measurements-they look at the whole picture.
How Do Doctors Predict If It Will Burst?
There’s no crystal ball, but there are tools. Two major scoring systems help guide decisions:
PHASES Score combines six factors: population, hypertension, age, aneurysm size, prior subarachnoid hemorrhage, and location. It gives you a 5-year rupture risk percentage. A score of 0-3 means a 3% risk. A score of 9-10? That’s 45%. If your score is 6 or higher, most experts recommend treatment.
Triple-S Model focuses on size, site, and shape. It’s especially useful after an aneurysm has grown. It can predict rupture risk over 6 months, 1 year, and 2 years-with 72% accuracy.
These aren’t guesses. They’re based on data from thousands of patients tracked over years. And they’re why some aneurysms get treated right away, while others are just watched.
Treatment Options: Clipping, Coiling, and Flow Diversion
If your aneurysm is high-risk, you have three main options. Each has trade-offs.
1. Surgical Clipping
This is the original method, first done in 1937. A neurosurgeon opens the skull, finds the aneurysm, and places a tiny titanium clip across its neck. This stops blood from flowing into it. Success rate? Around 95% immediate occlusion. Long-term cure? 88-92%.
Pros: Permanent fix. Low chance of needing another procedure.
Cons: Invasive. Requires a craniotomy. Recovery takes weeks. Risk of stroke or infection. Patients over 70 have 35% higher complication rates.
2. Endovascular Coiling
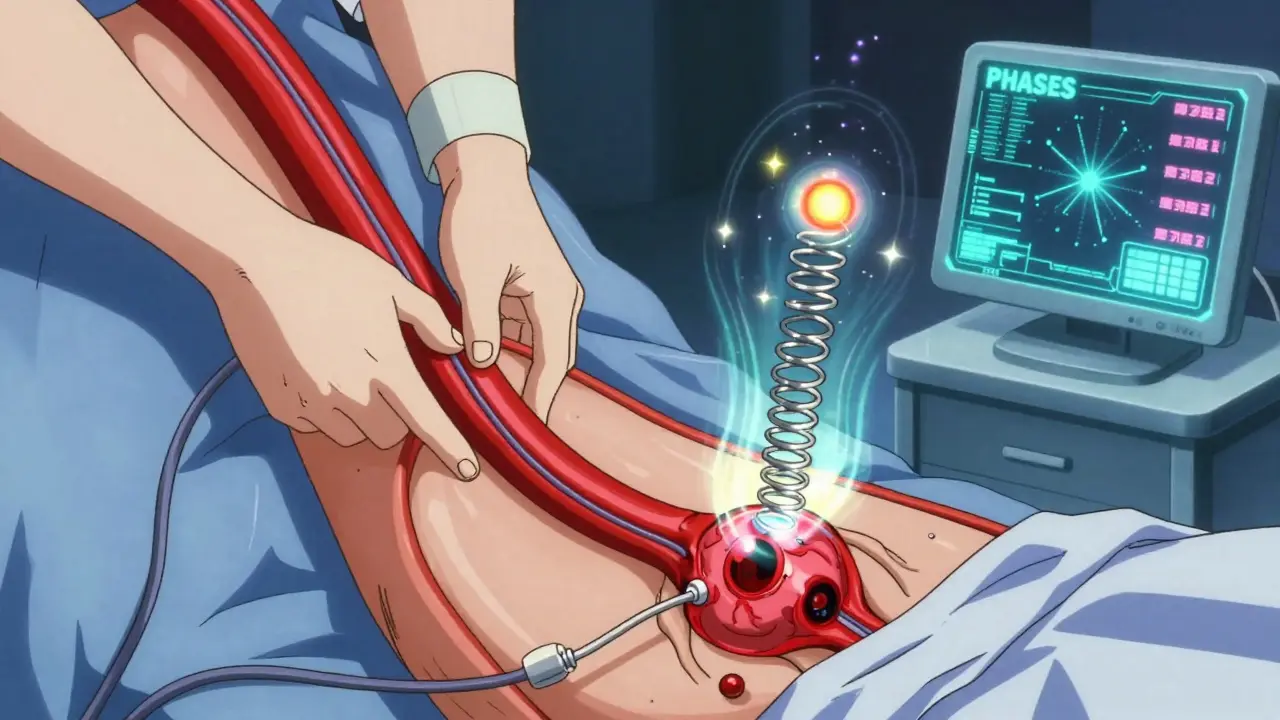
First done in 1991, this is a minimally invasive procedure. A catheter is threaded from the groin up to the brain. Tiny platinum coils are packed into the aneurysm, triggering a clot that seals it off. Modern success rates: 78-85% complete occlusion at 6 months.
Pros: No open surgery. Shorter hospital stay. Faster recovery. Lower 1-year mortality than clipping (8.1% vs 10.1%).
Cons: Higher chance of needing retreatment-15.7% over 12 years, compared to 6.2% for clipping. Not ideal for wide-necked aneurysms.
3. Flow Diversion
This is the newest approach, approved in 2011. A mesh stent (like the Pipeline Embolization Device) is placed across the artery’s opening. Blood is redirected away from the aneurysm, letting it slowly shrink and seal off. Used mostly for large or giant aneurysms, or those with wide necks.
Pros: Works where coiling can’t. 85.5% complete occlusion at 1 year in recent trials.
Cons: Requires blood thinners for months. Higher risk of delayed stroke. Morbidity rate is 5.2%.
What About the WEB Device?
For aneurysms at branch points (bifurcations), a newer device called the Woven EndoBridge (WEB) was approved in 2019. It looks like a tiny mesh cage that sits inside the aneurysm. In trials, it achieved 71.4% complete occlusion at one year. It’s especially useful for aneurysms that are hard to reach with coils or clips.
Choosing the Right Treatment
There’s no one-size-fits-all. Your decision depends on:
- Aneurysm shape and size. Wide neck? Flow diversion or WEB might be better.
- Location. Posterior circulation aneurysms (back of the brain) have 22% higher complication rates with clipping.
- Your age and health. If you’re over 70 or have heart disease, minimally invasive options are usually safer.
- Previous rupture. If you’ve had one rupture, your risk of another is over five times higher.
For many people with small, low-risk aneurysms, the best treatment is no treatment-at least not yet. The UCAS Japan study found that aneurysms under 5 mm in the anterior circulation had only a 0.2% chance of rupturing over five years. That’s lower than the risk of a car accident on your daily commute.
Medical Management: The Silent Hero
Treatment isn’t just surgery or coils. The most powerful tool for many people is lifestyle change.
- Blood pressure control. Target under 130/80 mmHg. This alone reduces rupture risk significantly.
- Quit smoking. Within two years, your rupture risk drops by 54%.
- Limit alcohol. Stick to under 14 drinks a week.
These aren’t suggestions. They’re medical necessities. For someone with a small aneurysm, these changes might be the only thing they ever need.
What Happens After Treatment?
Successful treatment cuts your 10-year re-rupture risk from 68% down to just 2.3%. That’s a massive difference.
But recovery isn’t just physical. Quality of life matters. Studies using the EQ-5D scale show that patients who get coiling report better daily function and less pain at one year than those who have surgery. That’s because recovery is faster, and complications like cognitive decline are less common.
Still, follow-up is critical. Even after successful coiling or flow diversion, you’ll need imaging-usually an MRA-every year to make sure the aneurysm stays sealed.
What’s Next in Research?
Science is catching up. The HUNT study found 17 genetic markers linked to aneurysm formation and rupture. That could one day lead to blood tests that predict risk before an aneurysm even forms.
Machine learning is being trained on hundreds of data points-shape, flow patterns, wall stress-to predict rupture better than current models. One algorithm now outperforms PHASES in accuracy, especially for small aneurysms.
These aren’t science fiction. They’re happening now. And they’ll change how we treat aneurysms in the next five years.
Final Thoughts: Knowledge Is Power
If you’ve been told you have a cerebral aneurysm, don’t panic. Most won’t rupture. But don’t ignore it either. Work with your neurologist or neurosurgeon. Get your PHASES score. Understand your size, shape, and location. Control your blood pressure. Quit smoking. Don’t drink heavily.
Treatment isn’t always the answer. Sometimes, the smartest thing you can do is watch-and live well while you do it.
Patrick Merrell
January 27, 2026 AT 22:54Smoking is the single worst thing you can do if you have an aneurysm. I knew a guy who smoked two packs a day and had a 4mm aneurysm. He quit cold turkey after his scare. Two years later, his follow-up scan showed it had shrunk. No surgery. No coils. Just willpower and clean air. If you’re still smoking, you’re playing Russian roulette with your brain.
Aurelie L.
January 28, 2026 AT 12:33I had a 5mm aneurysm found during a migraine scan. They told me to watch it. I cried for three days. Then I stopped drinking, started yoga, and now I check my BP every morning. It’s not a death sentence. It’s a wake-up call.
Joanna Domżalska
January 29, 2026 AT 20:27They say 'most don't rupture' but that's not comforting when you're the one in the 1 in 30. Also why is everyone acting like quitting smoking is some heroic act? It's basic. If you're not doing it, you're just lazy. And don't get me started on 'watch and wait'-that's just medical cowardice hiding behind statistics.
Faisal Mohamed
January 31, 2026 AT 05:17The PHASES score is fundamentally flawed because it fails to account for hemodynamic shear stress gradients in the arterial wall, which are now understood to be the primary biomechanical drivers of aneurysmal progression. The Triple-S model is more robust, but even that lacks integration of intraluminal flow dynamics derived from 4D-flow MRI. Until we move beyond size and location as proxies, we're just guessing with better charts.
Josh josh
January 31, 2026 AT 18:37so i got diagnosed last year with a 6mm thingy near my front brain thing and my doc said just chill and dont smoke and i did and now im alive and my wife says im a better husband cause i dont drink anymore lol
bella nash
February 1, 2026 AT 21:24It is imperative to underscore the clinical significance of lifestyle modification as a primary therapeutic modality in the management of unruptured cerebral aneurysms. The empirical evidence supporting blood pressure control and tobacco cessation is robust and statistically significant. Furthermore, the longitudinal outcomes data suggest that non-interventional management, when appropriately monitored, yields favorable prognostic outcomes in low-risk subpopulations.
Curtis Younker
February 3, 2026 AT 10:01Listen, I used to be a smoker, I used to drink like it was my job, and I had a 7mm aneurysm. I thought I was invincible. Then my mom had a rupture and didn’t make it. I quit smoking that day. Stopped drinking. Started walking 5 miles a day. My BP is 118/76 now. My last scan showed the aneurysm hasn’t grown in 18 months. It’s not magic. It’s just choices. You can do this. I’m not saying it’s easy-I’m saying it’s worth it. Your brain is worth fighting for.
Shawn Raja
February 4, 2026 AT 07:41Oh wow, so now we’re telling people to quit smoking because a balloon in their head might pop? Next they’ll say drinking coffee causes spontaneous combustion. Look, if your aneurysm is small and you’re not a smoker, maybe stop obsessing over it. You’re more likely to die from a falling coconut than a 4mm aneurysm. Let people live. Or at least let them have one cigarette.
Allie Lehto
February 4, 2026 AT 12:59im so glad this post exists i had no idea about the web device and i think its so cool that they can just put a little mesh cage in there like a tiny net to catch the bleed before it happens?? i quit smoking 3 months ago and my dr said my risk dropped already so im proud of myself even though i still forget to take my bp pills sometimes lol