What Deep Brain Stimulation Actually Does for Parkinson’s
Deep Brain Stimulation, or DBS, isn’t a cure for Parkinson’s. It doesn’t stop the disease from progressing. But for many people, it changes everything. If your tremors won’t quit, your meds cause wild swings between freezing up and uncontrollable movements, or you’re tired of swallowing pills every hour - DBS can help. It works by sending tiny electrical pulses to specific spots in the brain that control movement. These pulses don’t kill brain cells. They don’t remove anything. They just quiet down the noisy signals that cause Parkinson’s symptoms.
The electrodes are placed in one of two areas: the subthalamic nucleus (STN) or the globus pallidus interna (GPi). Both work well, but they have different strengths. STN tends to let people cut back on their levodopa dose by 30-50%. That means fewer side effects like nausea, dizziness, or sudden urges to gamble or eat. GPi, on the other hand, is better at smoothing out the jerky, involuntary movements called dyskinesias. If you’re struggling more with those than with OFF periods, GPi might be the better pick.
Modern systems like Medtronic’s Percept™ PC and Boston Scientific’s Vercise™ Genus™ can actually sense what’s happening in your brain. They pick up on abnormal brainwave patterns - especially the beta waves between 13-35 Hz - that spike when you’re stiff or slow. Some newer devices use that data to adjust stimulation automatically. It’s like having a smart thermostat for your brain.
Who Really Benefits from DBS?
Not everyone with Parkinson’s is a candidate. The biggest red flag? If your symptoms don’t improve when you take levodopa, DBS won’t help much. Studies show people with atypical parkinsonism - like progressive supranuclear palsy or multiple system atrophy - get less than 10% improvement. But if you’ve had Parkinson’s for at least five years and still get strong relief from levodopa, you’re likely a good fit.
Doctors look for a clear 30% or better improvement in your motor score (UPDRS Part III) when you’re on medication versus off. That’s not just a number - it’s your real-life ability to walk, button shirts, or get out of a chair. If you’ve lost that response, DBS won’t bring it back.
Another key factor: cognitive health. If your memory or thinking skills are already slipping - say, your MoCA score is below 21 or your MMSE is under 24 - DBS can make things worse. You might struggle more with planning, focusing, or finding words. One patient on Reddit said, “My tremors are gone, but now I can’t plan my meals without writing everything down.” That’s not rare. Neuropsychological testing isn’t optional. It’s mandatory.
Age isn’t a hard cutoff, but most candidates are under 70. Older patients can still do well, but recovery takes longer, and risks like infection or bleeding go up slightly. The real issue isn’t age - it’s overall health. If you have heart disease, diabetes, or poor lung function, surgery becomes riskier.
The Surgery: What Happens From Start to Finish
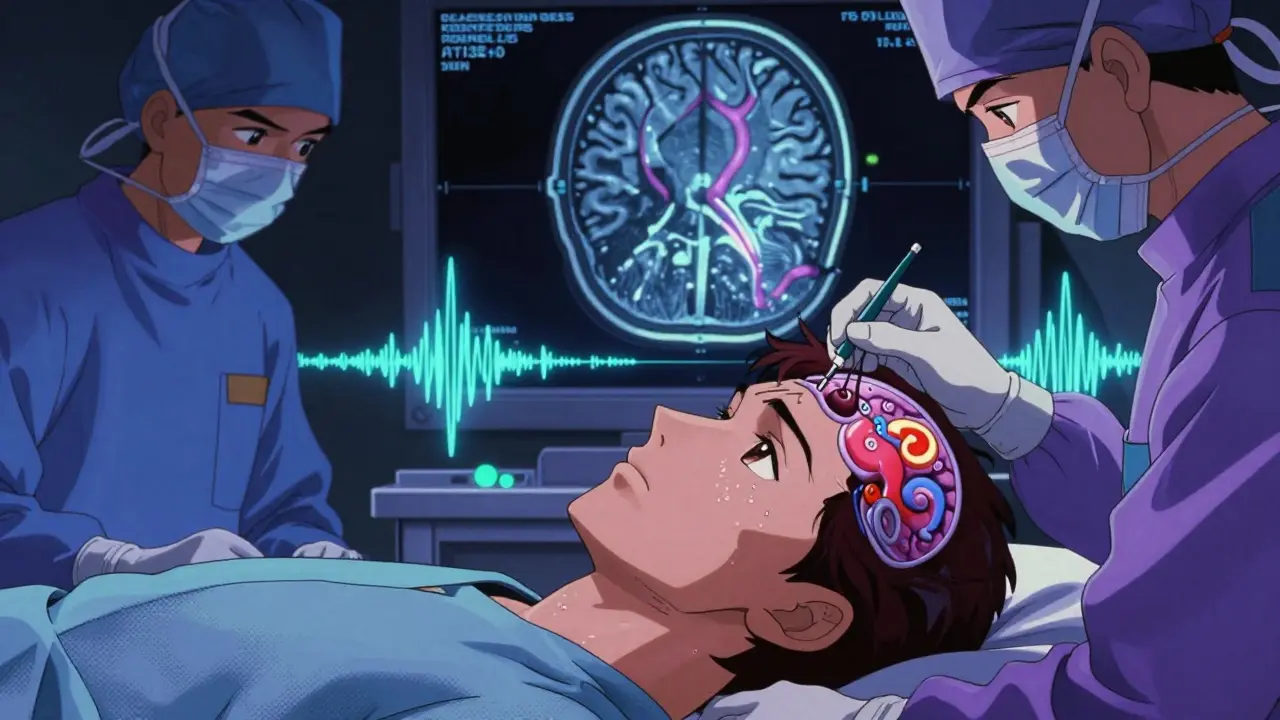
DBS surgery isn’t done under full anesthesia. You’re awake - mostly. You’ll be sedated enough to feel calm, but you need to be alert so the team can test your responses during the procedure. That’s how they know they’ve hit the right spot. If you twitch when they zap a certain area, they know they’re close. If your speech gets slurred, they back off.
Before surgery, you get a high-resolution 3T MRI to map your brain. A metal frame is attached to your skull to hold everything perfectly still. Then, thin wires - just 1.27mm wide - are threaded through small holes in your skull. Each one goes to a target deep inside the brain. The whole process takes 3 to 6 hours. Most people go home the next day.
After surgery, you wait 2-4 weeks for swelling to go down before the device is turned on. That’s when the real work begins. The first programming session can take 2-3 hours. You’ll sit in a chair, hold a tablet, and describe how you feel as the doctor adjusts voltage, frequency, and which contacts on the electrode are active. It’s not a one-time fix. Most people need 6 to 12 months of fine-tuning. Some come in monthly at first. Others get remote programming via Bluetooth from their neurologist’s office.
What You Can Expect - and What You Can’t
DBS is amazing for tremors, stiffness, and slowness. Most patients see a 60-80% drop in OFF time. Dyskinesias shrink by up to 80%. Medication doses often drop significantly. In the EARLYSTIM trial, people who got DBS early reported a 23-point improvement in quality of life on the PDQ-39 scale - nearly double the gain of those who stuck with meds alone.
But here’s what it won’t fix: balance problems, freezing of gait, speech issues, or swallowing difficulties. These are called axial symptoms, and they respond poorly to DBS - often only 20-30% improvement at best. Depression and anxiety might improve if they’re tied to motor fluctuations, but not always. And DBS doesn’t stop dementia. If you’re already having memory trouble, it could get worse.
One patient wrote on a Parkinson’s forum: “I thought DBS would stop the disease. It didn’t. It just gave me back my days.” That’s the right mindset. DBS doesn’t reverse Parkinson’s. It gives you back control over the symptoms that respond to levodopa. If you expect magic, you’ll be disappointed. If you expect relief - real, measurable, life-changing relief - you’re likely to get it.
Cost, Risks, and Hidden Challenges
DBS isn’t cheap. In the U.S., the total cost ranges from $50,000 to $100,000. Medicare and most private insurers cover it if you meet criteria, but getting approval can take 3-6 months. You’ll need documentation showing you’ve tried and failed on multiple medication regimens.
Surgical risks are low but real. About 1-3% of people have bleeding in the brain. That can cause stroke-like symptoms - weakness, speech loss, confusion. Infection happens in 3-5% of cases. Sometimes the wires shift or break. Hardware issues like broken leads or faulty batteries happen in 5-15% of patients over time. You might need a second surgery to fix it.
Battery life depends on the device. Older models last 3-5 years. Newer rechargeable ones last 9-15 years. But you still have to plug them in every few days. Some patients forget. Others hate the routine. One man on a support group said, “I’d rather have the tremors than remember to charge my brain.”
And then there’s the emotional side. Many people feel let down when non-motor symptoms don’t improve. Fatigue, sleep problems, constipation - those don’t vanish with DBS. If you weren’t warned about that, you might feel like the surgery failed. That’s why multidisciplinary teams matter. Neurologists, neurosurgeons, neuropsychologists, and therapists need to talk before you sign the consent form.
Who Should Avoid DBS?
There are clear reasons to say no. If your Parkinson’s isn’t responsive to levodopa, skip it. If you have dementia, severe depression, or uncontrolled anxiety, DBS could make things worse. If you’re not willing to commit to long-term follow-ups - monthly visits, keeping symptom diaries, adjusting to new settings - you’re not ready.
People with other neurological conditions - like ALS, MS, or stroke-related parkinsonism - usually don’t benefit. And if you’re hoping for a miracle, you’ll be disappointed. DBS isn’t for everyone. But for the right person, it’s life-changing.
Right now, only 1-5% of eligible Parkinson’s patients get DBS. Most are never even referred. Too many wait until they’re stuck in bed, unable to walk, or drowning in pills. The best time to consider DBS is when you still have good mobility - but your meds are starting to fail. That’s when the gains are biggest.
The Future of DBS: Smarter, Earlier, Personalized
The field is moving fast. The latest FDA-approved devices, like Medtronic’s Percept™ PC, don’t just stimulate - they record brain signals. That means doctors can see exactly when your symptoms flare and adjust stimulation in real time. Early results show 27% better control than old-school DBS.
Researchers are testing DBS in people with just three years of Parkinson’s. The EARLYSTIM-2 trial is asking: What if we intervene before motor complications become severe? Early data suggests younger patients recover faster and have fewer cognitive side effects.
And it’s not just about the brain anymore. Scientists are looking at genetics. People with the LRRK2 mutation respond better to DBS - 15% more improvement. Future screenings might include genetic tests alongside cognitive and motor evaluations. Imagine a future where your DBS settings are tailored not just to your symptoms, but to your DNA.
Apple Watch apps that track tremors could one day sync with your DBS device. Your phone could alert your doctor when your symptoms worsen overnight. This isn’t sci-fi. It’s happening.
Final Thoughts: Is DBS Right for You?
If you’ve been on levodopa for five or more years and still get good relief from it - but the effects are fading, or the side effects are unbearable - DBS is worth exploring. Don’t wait until you’re trapped in your body. Talk to a movement disorder specialist. Get a neuropsych eval. See what your MRI shows. Ask about the team’s experience. Centers that do more than 50 DBS surgeries a year have fewer complications.
DBS isn’t a magic button. But for the right person, it’s the closest thing to one.
Is DBS a cure for Parkinson’s disease?
No, DBS is not a cure. It does not stop Parkinson’s from progressing. It only treats motor symptoms that respond to levodopa, such as tremors, stiffness, slowness, and dyskinesias. It does not improve balance, speech, swallowing, or cognitive decline. Patients often describe it as giving back control over their symptoms, not reversing the disease.
How long does it take to see results after DBS surgery?
You won’t feel the full effects right away. After surgery, you need 2-4 weeks for swelling to go down. The device is then turned on, but programming takes time. Most patients need 6-12 months of regular adjustments to find the optimal settings. Improvements in motor symptoms often become clear within weeks, but fine-tuning for balance, speech, and medication timing can take much longer.
Can DBS help with non-motor symptoms like depression or sleep problems?
Sometimes, but not reliably. If your depression or sleep issues are tied to motor fluctuations - like being stuck in an OFF state for hours - DBS can help indirectly by reducing those OFF periods. But DBS doesn’t directly treat anxiety, fatigue, constipation, or dementia. Some patients report mood changes after surgery, either improvement or worsening. That’s why neuropsychological screening before surgery is critical.
What’s the difference between STN and GPi targets?
STN (subthalamic nucleus) usually allows for greater reduction in levodopa dose - often 30-50%. This means fewer medication side effects. GPi (globus pallidus interna) is better at reducing dyskinesias and may cause fewer cognitive or mood side effects. Both improve motor symptoms equally, but the choice depends on your biggest problem: medication side effects (choose STN) or involuntary movements (choose GPi).
How often do DBS batteries need replacing?
Non-rechargeable batteries last 3-5 years and require minor surgery to replace. Rechargeable systems, like those from Medtronic and Boston Scientific, last 9-15 years. But you must charge them every few days. Some patients find the routine frustrating, while others prefer fewer surgeries. Battery life depends on stimulation settings - higher voltage and frequency drain power faster.
Why are so few Parkinson’s patients getting DBS?
Many patients are never referred. Others wait too long, until their symptoms are too advanced or cognitive decline has started. Doctors sometimes assume patients are too old or too sick. Insurance approvals can take months. And many patients don’t know DBS exists - they think it’s only for tremor or for people who are “severe.” In reality, the best candidates are those who still respond well to levodopa but struggle with its side effects. That’s often people in their 50s or early 60s - not the very elderly.
Can I have an MRI after DBS surgery?
Yes - but only under strict conditions. Most modern DBS systems are MRI-conditional, meaning you can have a 1.5T or 3T MRI if specific safety settings are used. The device must be turned off, and the MRI must be done with special protocols. Always inform the radiology team you have a DBS implant. Some older systems are not MRI-safe at all. Check with your device manufacturer and neurologist before scheduling any scan.
Does DBS affect speech or swallowing?
It can. Some patients develop slurred speech, reduced volume, or difficulty swallowing - especially if the electrodes are too close to areas controlling those functions. This is often reversible by adjusting stimulation settings. Speech therapy is recommended after surgery. If speech problems start after programming, tell your neurologist immediately - they can often fix it without surgery.
What happens if I stop using the DBS device?
If you turn off or remove the device, your Parkinson’s symptoms will return to their pre-surgery state - no worse, no better. DBS doesn’t change the underlying disease. It only masks symptoms while it’s active. Some patients choose to turn it off temporarily if they’re having side effects. The system is reversible, which is one of its biggest advantages over older lesioning procedures like pallidotomy.
Are there alternatives to DBS for Parkinson’s?
Yes. Focused ultrasound (Exablate Neuro) is a non-invasive option approved for tremor-dominant Parkinson’s, but it’s only done on one side of the brain and doesn’t help with other symptoms like slowness or dyskinesias. Lesioning surgeries (pallidotomy, thalamotomy) are permanent and carry higher risks of permanent side effects. Medication adjustments, physical therapy, and wearable tech (like smartwatches that track tremors) are supportive but not replacements for DBS in advanced cases.
Sahil jassy
December 17, 2025 AT 18:01Kathryn Featherstone
December 18, 2025 AT 13:29Nina Stacey
December 18, 2025 AT 17:12Marsha Jentzsch
December 19, 2025 AT 03:40Kevin Motta Top
December 21, 2025 AT 02:00Aadil Munshi
December 21, 2025 AT 05:17William Storrs
December 22, 2025 AT 23:23Dorine Anthony
December 23, 2025 AT 00:51Gloria Parraz
December 24, 2025 AT 08:48Frank Drewery
December 25, 2025 AT 08:31Danielle Stewart
December 26, 2025 AT 01:11Alisa Silvia Bila
December 26, 2025 AT 06:45James Stearns
December 27, 2025 AT 10:49mary lizardo
December 28, 2025 AT 06:32