For decades, doctors told us: take vitamin D to protect your bones. It’s simple, logical, and seemed backed by science. But today, the story isn’t so clear. High-dose vitamin D supplements? They might not help - and could even hurt. Meanwhile, people with low levels are still at real risk. So what’s the truth? And what should you actually do for your bones?
Why Vitamin D Matters for Bones
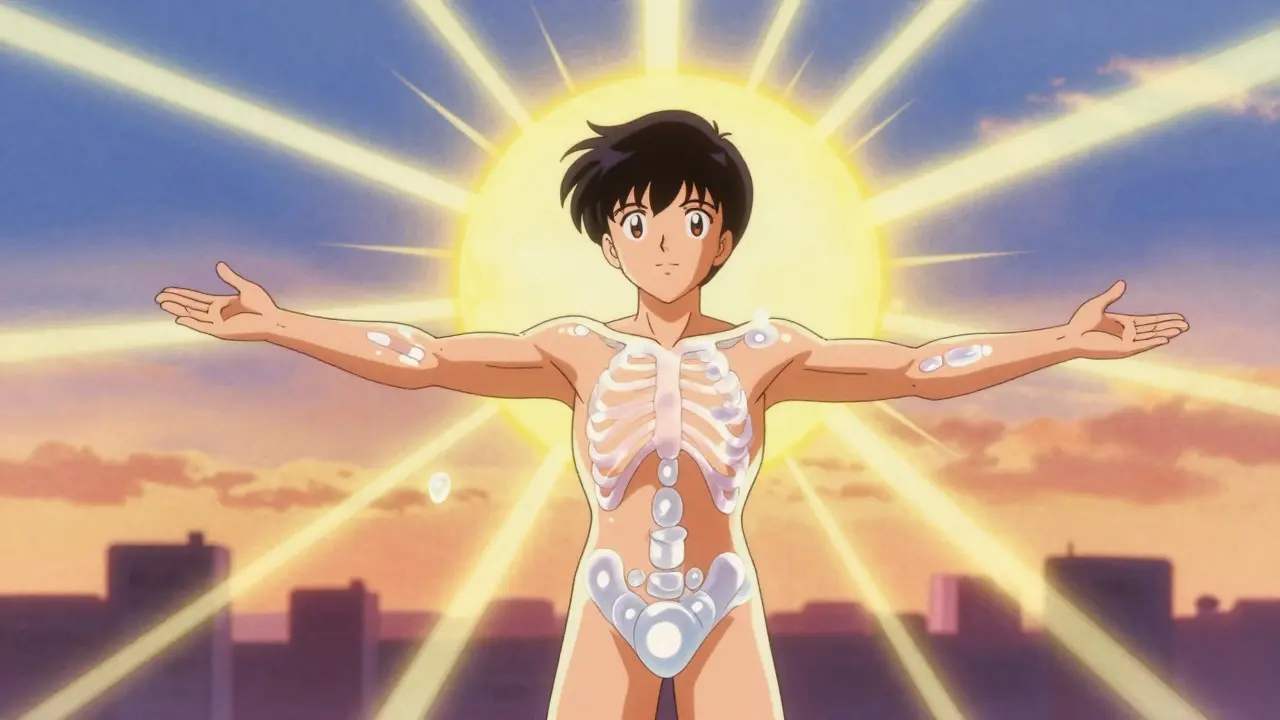
Vitamin D doesn’t build bone directly. It’s the gatekeeper for calcium. Without enough vitamin D, your body absorbs only 10-15% of the calcium you eat. With enough, that jumps to 60-80%. That’s the difference between weak, porous bones and strong, dense ones. It also helps your muscles work better, reducing the chance of falls - a major cause of fractures in older adults.
The link between vitamin D and bone health was first proven in the early 1900s when researchers found it cured rickets, a disease that softened children’s bones. Today, we know it’s just as critical for adults. But now we’re learning that more isn’t always better.
What’s the Right Level of Vitamin D?
The standard blood test measures 25-hydroxyvitamin D - or 25(OH)D. For years, the cutoff for deficiency was 20 ng/mL. Below that, you were told to take supplements. But recent studies are shaking that up.
The Endocrine Society says you need at least 30 ng/mL for optimal bone health. But the VITAL trial, a massive study led by Harvard Medical School, found no extra bone protection above 20 ng/mL in healthy adults. In fact, people with levels between 20 and 30 ng/mL had the same fracture rates as those with levels above 30.
Here’s the twist: if your level is below 20, fixing it helps. If you’re already above 20, taking more doesn’t improve your bone density. And if you go way over - say, 10,000 IU a day - you might actually lose bone mass. A 2020 JAMA study showed people taking 4,000 or 10,000 IU daily had lower bone density in their wrists and shins compared to those taking just 400 IU.
The Supplementation Debate
Most guidelines still recommend 600-800 IU daily for adults. But the Endocrine Society suggests 1,500-2,000 IU to keep levels above 30 ng/mL. So which is right?
The answer depends on your starting point. A 2020 meta-analysis in the Journal of Bone and Mineral Research found that in people with low baseline vitamin D levels (below 14.2 pmol/L), taking 2,000 IU daily helped slow bone loss and slightly improved spine density. But for people with normal levels, there was zero benefit.
Even more telling: a 2023 meta-analysis in Nutrients showed that calcium and vitamin D together reduced hip fracture risk by 30% - but only when vitamin D was under 400 IU per day. At higher doses, the benefit disappeared. That’s not a typo. More vitamin D didn’t mean better bones. It meant no change - or worse.
Dr. Meryl LeBoff, lead researcher on the VITAL trial, put it bluntly: “Healthy older adults taking 2,000 IU daily had no fewer fractures than those on placebo.”
Who Actually Needs Supplements?
Not everyone. But some groups are at real risk:
- People with dark skin - melanin reduces vitamin D production from sunlight.
- Those living north of 37° latitude - in winter, the sun’s rays aren’t strong enough to make vitamin D.
- People over 65 - skin becomes less efficient at making vitamin D.
- People with obesity (BMI ≥30) - vitamin D gets trapped in fat tissue, lowering blood levels by up to 57%.
- Those with malabsorption conditions like Crohn’s or celiac disease.
If you fit one or more of these, get tested. Don’t guess. A simple blood test can tell you if you’re below 20 ng/mL. If you are, supplementing makes sense. If you’re not - you’re probably fine.
Choosing the Right Supplement
Not all vitamin D is the same. There are two forms: D2 (from plants) and D3 (from animals and sunlight). D3 is the winner - it raises blood levels 87% more effectively than D2, according to a 2011 study in the Journal of Clinical Endocrinology & Metabolism.
Stick with D3. Look for supplements that specify “cholecalciferol.” Avoid D2 unless your doctor recommends it for a specific reason.
And don’t assume your label is accurate. ConsumerLab’s 2022 review found that 15% of vitamin D supplements contained less than 90% of the labeled amount. One brand had only 72% of what it claimed. Another exceeded its label by 128%. Stick with trusted brands - or better yet, choose ones with USP or NSF certification.
Timing and Absorption Matter
Vitamin D is fat-soluble. That means it needs fat to be absorbed. Taking it on an empty stomach? You’re wasting most of it.
A 2015 study showed that taking vitamin D with your largest meal - usually dinner - boosted absorption by 56.7%. That’s not a small difference. It’s the difference between getting 100 IU and 156 IU from a 1,000 IU pill.
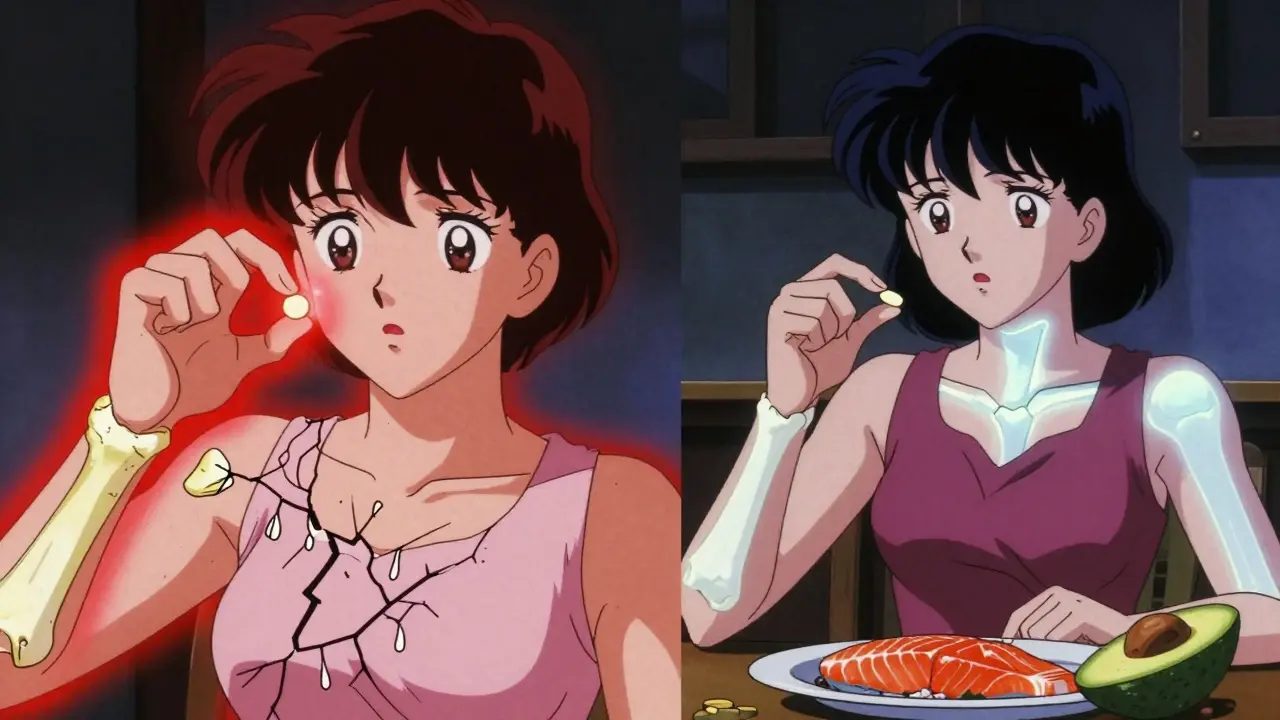
Don’t take it with your morning coffee. Take it with your evening salmon, avocado toast, or cheese. Fat makes it work.
Calcium Still Matters - But Don’t Overdo It
Vitamin D helps you absorb calcium. But calcium itself is the building block. You still need enough.
The recommended daily intake is 1,000-1,200 mg for adults over 50. You can get this from dairy, leafy greens, fortified foods, or supplements. But if you’re taking high-dose calcium supplements (like 1,000 mg a day) with vitamin D, you might be setting yourself up for problems.
Some people report severe constipation from calcium-vitamin D combos like Citracal. Switching to liquid D3 drops and getting calcium from food often solves the issue. And again - if your vitamin D is already normal, extra calcium won’t help your bones. It might even raise your risk of kidney stones.
What About High-Dose Supplements?
Some people swear by 5,000 or 10,000 IU daily. Reddit threads are full of stories: “My bone density improved!” or “It got worse.”
But science says this: high doses aren’t magic. They’re risky. The JAMA study showed clear bone loss at 10,000 IU daily. And the VITAL trial found no benefit at 2,000 IU for people without deficiency.
If you’re taking more than 4,000 IU daily without medical supervision, you’re in uncharted territory. The upper limit set by the Institute of Medicine is 4,000 IU for adults. That’s not a suggestion - it’s the ceiling for safety.
Testing and Timing
Don’t test right after starting a supplement. It takes about 3 months for your blood levels to stabilize. Test too soon, and you’ll get a false reading.
If you start 2,000 IU a day in January, wait until April to get your blood drawn. Then adjust based on results - not on how you feel. Vitamin D doesn’t give you energy or fix fatigue in healthy people. It just helps your bones absorb calcium.
What’s the Bottom Line?
Here’s what the evidence says today:
- If your 25(OH)D level is below 20 ng/mL - supplement with 1,000-2,000 IU of D3 daily until you reach 20-30 ng/mL.
- If your level is 20 ng/mL or higher - no need to supplement unless you’re at high risk for falls or fractures. Your diet and sun exposure are probably enough.
- Avoid doses over 4,000 IU daily unless under medical supervision. Higher doses don’t improve bone density - they can lower it.
- Take vitamin D with your biggest meal - preferably dinner - to maximize absorption.
- Choose D3 over D2, and pick a certified brand to ensure accuracy.
- Get calcium from food first. Supplements should fill gaps, not replace meals.
The old advice - “take vitamin D for strong bones” - is outdated. It’s not about taking more. It’s about taking the right amount for your body.
What’s Next?
Research is moving toward personalization. The NIH now says vitamin D needs should be based on your baseline level, BMI, and even your genes. Upcoming studies like the D-Health Trial (2024) will test monthly high-dose regimens (60,000 IU) versus placebo in 21,000 older Australians. We may learn that less frequent, higher doses work better - or that they’re just as risky.
For now, the safest, most evidence-based approach is simple: test first, supplement only if needed, and never go beyond 4,000 IU without a doctor’s guidance. Your bones aren’t asking for more. They’re asking for just enough.
Is vitamin D deficiency common?
Yes, especially in older adults, people with dark skin, those living far from the equator, and individuals with obesity. Studies estimate up to 40% of adults in the U.S. have levels below 20 ng/mL. But many don’t know it - symptoms like fatigue or muscle weakness are often mistaken for aging or stress.
Can I get enough vitamin D from sunlight alone?
It depends. Fair-skinned people can make enough vitamin D in 10-15 minutes of midday sun on arms and legs, 2-3 times a week. But in winter, at northern latitudes, or if you wear sunscreen or cover your skin, you won’t make enough. Plus, older adults and people with darker skin need more exposure. For most people, sunlight alone isn’t reliable year-round.
Do I need to take vitamin D with calcium?
Only if you’re not getting enough calcium from food. Most people who eat dairy, leafy greens, or fortified foods get enough. If you’re deficient in both, combining them helps reduce fracture risk - but only at low to moderate doses (under 400 IU vitamin D). High-dose combinations offer no extra benefit and may cause side effects like constipation.
Can too much vitamin D hurt my bones?
Yes. Studies show that daily doses of 4,000 IU or more - especially 10,000 IU - can lead to lower bone mineral density over time. This happens because excess vitamin D may speed up bone turnover, breaking down bone faster than it rebuilds. The body doesn’t store vitamin D safely at very high levels - it becomes toxic to bone tissue.
What’s the best form of vitamin D supplement?
Vitamin D3 (cholecalciferol) is the most effective form. It’s identical to what your skin makes from sunlight. Avoid D2 (ergocalciferol) unless prescribed. Look for supplements with USP or NSF certification to ensure accurate dosing. Liquid drops taken with food are often easier to absorb than pills.
Should I take vitamin D if I have osteoporosis?
Yes - but only if your blood level is low. If your 25(OH)D is below 20 ng/mL, supplementing to reach 20-30 ng/mL is part of standard treatment. But vitamin D alone won’t reverse osteoporosis. It’s used alongside medications like bisphosphonates or denosumab. High doses (over 2,000 IU) aren’t recommended unless your doctor specifically advises it.
Donna Hammond
December 16, 2025 AT 16:12Finally, someone laid this out clearly. I used to take 5,000 IU daily because I thought more was better. Turned out my levels were already at 28. No benefit. Just wasted money and made me paranoid about kidney stones. Now I get tested every year and only supplement if needed. Simple. Smart.
Also, taking it with dinner? Game changer. I used to take it with breakfast and felt nothing. Now I take it with my salmon and avocado toast - and honestly, my legs don’t cramp at night anymore.
PS: Always get USP-certified. I learned that the hard way after buying some random brand off Amazon that had half the labeled dose.
Richard Ayres
December 17, 2025 AT 22:55Thank you for this meticulously researched summary. The disconnect between public perception and clinical evidence regarding vitamin D supplementation is both concerning and fascinating. The VITAL trial findings, in particular, underscore the necessity of evidence-based rather than assumption-driven health practices.
It is worth noting that while high-dose supplementation may appear beneficial in isolated anecdotal reports, population-level data consistently fails to support such interventions in non-deficient individuals. The physiological mechanisms underlying bone turnover and calcium homeostasis are complex and should not be oversimplified.
For clinicians, this reinforces the importance of individualized care - not blanket recommendations.
Sheldon Bird
December 19, 2025 AT 15:30Yessss!! This is the kind of info we need more of 😊
I was taking 4,000 IU every day like it was vitamins candy. Then I got tested - 32 ng/mL. No need. Cut it to 800 IU with dinner. My knees stopped creaking. No magic, just science.
Also - D3 only. D2 is like using a spoon to dig a tunnel. 🤦♂️
And yeah, buy certified. I learned that after one brand gave me 72% of what it said. That’s not a supplement, that’s a scam.
sharon soila
December 20, 2025 AT 21:13There is a deep truth here. The body does not need excess. It needs balance.
For centuries, humans lived without supplements. They got what they needed from sun, food, and rhythm. We have lost that rhythm. We think more is better because we live in a world of abundance and advertising.
But bones are not built by pills. They are built by harmony - sunlight, movement, nutrition, rest.
Supplements are tools, not crutches. Use them wisely. Test before you take. And never forget: nature knows better than the bottle.
nina nakamura
December 22, 2025 AT 06:36Hamza Laassili
December 23, 2025 AT 13:02Rawlson King
December 25, 2025 AT 03:48Let me be blunt: this article is dangerously naive. You cite VITAL and JAMA, but ignore the broader epidemiological data showing consistent correlation between higher vitamin D levels and reduced fracture risk across multiple continents. You reduce a multifactorial physiological process to a binary: 'if you're above 20, you're fine.' That's not science - it's reductionist dogma.
And the suggestion to avoid supplementation unless deficient? That’s a recipe for widespread osteoporosis in aging populations, especially where sun exposure is minimal. You're ignoring the reality of modern life.
Don't confuse 'no additional benefit in healthy adults' with 'no benefit at all.'
Cole Newman
December 26, 2025 AT 13:10