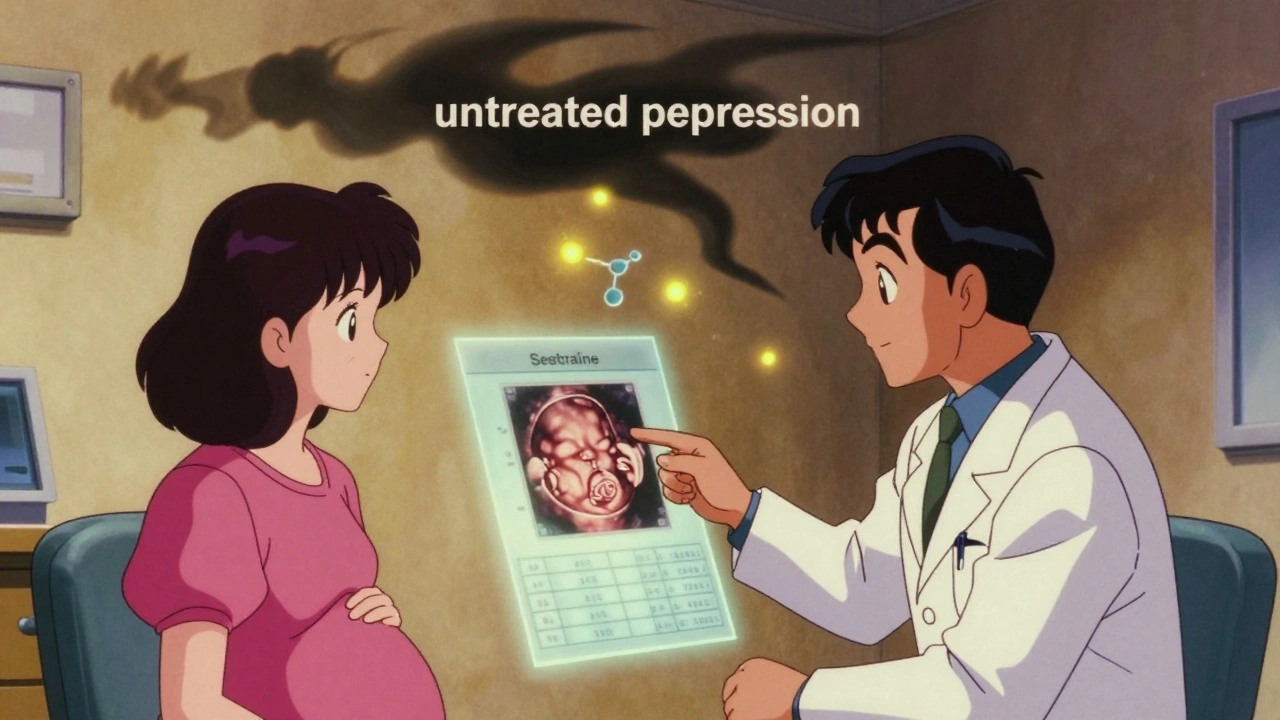
When you’re pregnant and struggling with depression, the question isn’t just whether to take antidepressants-it’s whether not taking them could be riskier. Many women worry about harming their baby. But the real danger might be leaving depression untreated.
Depression During Pregnancy Is Common-and Dangerous
About 1 in 7 pregnant people in the U.S. experience depression. That’s not rare. It’s one of the most frequent complications of pregnancy. And untreated, it doesn’t just affect your mood. It affects your baby’s health too.Studies show women with untreated depression are 40% more likely to have a preterm birth, 30% more likely to have a baby with low birth weight, and 25% more likely to develop preeclampsia. They’re also 50% less likely to attend regular prenatal visits. Depression can make it hard to eat well, sleep, or even get out of bed-things that directly impact fetal development.
And the risks don’t stop at birth. Between 2017 and 2019, mental health conditions were the leading cause of pregnancy-related deaths in the U.S., accounting for nearly a quarter of all cases. Suicide and overdose, often linked to unmanaged depression, are major contributors. The choice isn’t between medication and safety-it’s between medication and serious, sometimes deadly, consequences.
Which Antidepressants Are Considered Safe?
Not all antidepressants are the same when you’re pregnant. The most commonly prescribed and best-studied are SSRIs-selective serotonin reuptake inhibitors. These include sertraline (Zoloft), citalopram (Celexa), escitalopram (Lexapro), and fluoxetine (Prozac).Among these, sertraline is the top choice for most doctors. Why? Because it has the most data showing it doesn’t increase the risk of birth defects, growth problems, or long-term developmental issues. Over 5 million births have been studied, and when researchers controlled for the fact that women taking SSRIs often have depression (which itself carries risks), the medication didn’t add extra danger.
There’s one exception: paroxetine (Paxil). It’s linked to a higher chance of heart defects in babies-about 1.5 to 2 times higher than other SSRIs. If you’re on paroxetine and planning pregnancy, talk to your doctor about switching before conception. If you’re already pregnant, don’t stop cold turkey-work with your provider to switch safely.
Serotonin-norepinephrine reuptake inhibitors (SNRIs) like venlafaxine are also used, but there’s less data. Tricyclic antidepressants are an option too, but they’re not first-line because they come with more side effects and less research.
What About Birth Defects?
Early studies raised alarms. Some suggested SSRIs might slightly increase the risk of major birth defects. But those studies didn’t account for something critical: the mother’s mental illness.When researchers compared women with depression who took SSRIs to women with depression who didn’t, the difference vanished. One large 2018 meta-analysis found that the risk of major congenital anomalies dropped from 1.25 to 1.04 when only women with diagnosed psychiatric conditions were included. That means the depression itself-not the medicine-was likely driving the small uptick in risk.
The Society for Maternal-Fetal Medicine (SMFM) summed it up clearly in July 2025: “The available data consistently show that SSRI use during pregnancy is not associated with congenital anomalies, fetal growth problems, or long-term developmental problems.”
Neonatal Adaptation Syndrome: What to Expect After Birth
Some babies exposed to SSRIs in the last trimester may have temporary symptoms after birth. This is called neonatal adaptation syndrome (or sometimes, neonatal withdrawal). About 30% of these infants show signs like jitteriness, mild breathing trouble, or feeding difficulties.Here’s the good news: these symptoms are not dangerous. They usually go away within 48 hours to two weeks. No long-term harm has been linked to them. And they’re far less common than the risks of untreated depression.
Doctors don’t recommend avoiding SSRIs because of this. Instead, they prepare for it. If you’re taking an SSRI in your third trimester, your care team will watch your baby closely after birth. Most babies need nothing more than extra feeding support and time.
Fluoxetine and the PPHN Question
Fluoxetine (Prozac) has been studied for a rare condition called persistent pulmonary hypertension of the newborn (PPHN). This is when a baby’s lungs don’t adjust properly after birth, making breathing hard.The risk is low. In babies not exposed to SSRIs, PPHN happens in about 2 to 3 out of every 1,000 births. With fluoxetine, it’s about 5 to 6 per 1,000. That’s a small increase-but still rare. And again, the risk of PPHN is far lower than the risk of complications from untreated depression.
Because of this, some doctors prefer sertraline over fluoxetine, especially if you’re in your third trimester. But if fluoxetine has worked well for you before pregnancy, switching isn’t always necessary. Your doctor will weigh your personal history against the numbers.
What Happens If You Stop Taking Your Medication?
Many women stop antidepressants as soon as they find out they’re pregnant. It’s understandable. But the data shows it’s risky.One study found that 68% of pregnant women who stopped their antidepressants had a depression relapse. Only 26% of those who continued did. That’s a huge difference.
And it’s not just about mood. Relapse increases the chance of preterm birth, low birth weight, and poor prenatal care. It can also lead to thoughts of self-harm or suicide.
Even worse, a 2025 study in JAMA Network Open found that nearly half of pregnant women stopped refilling their antidepressant prescriptions compared to the year before pregnancy. And there was no increase in therapy or other support. That means many women are going without any treatment at all.
Stopping abruptly can also cause withdrawal symptoms-dizziness, nausea, anxiety, even electric-shock sensations. That’s why doctors never recommend stopping cold turkey. If you want to change your medication, do it slowly and under supervision.
Non-Medication Options Are Part of the Plan
Medication isn’t the only tool. Cognitive behavioral therapy (CBT) has been shown to be just as effective as SSRIs for mild to moderate depression during pregnancy. Exercise, sunlight, sleep hygiene, and social support also help.But here’s the catch: therapy takes time, money, and access. Not everyone can get weekly sessions. And for severe depression, therapy alone often isn’t enough.
The best approach? Combine them. If you’re on medication, add therapy. If you’re trying therapy first, have a plan to start medication if symptoms don’t improve. Your obstetrician and psychiatrist should work together to make that happen.
Why the Confusion? The FDA Panel Controversy
In July 2025, an FDA expert panel released a report that sent shockwaves through the medical community. It raised concerns about SSRIs in pregnancy that many doctors felt were misleading.ACOG responded quickly. Their president called the panel “alarmingly unbalanced.” He pointed out that only one of the ten panelists emphasized how vital these medications are for preventing death and disability from untreated depression.
The problem? The panel didn’t account for the real-world context. It focused on small statistical risks without weighing them against the proven dangers of depression. The result? Fear. And fear leads women to stop treatment-even when it’s the safest option.
Leading organizations like SMFM and ACOG stand by the evidence: SSRIs are safe. The benefits almost always outweigh the risks.
What Should You Do?
If you’re pregnant or planning to be, and you’re on antidepressants:- Don’t stop without talking to your doctor.
- If you’re on paroxetine, ask about switching to sertraline or citalopram.
- If you’re not on medication but struggling with depression, don’t wait. Talk to your OB or a psychiatrist.
- Ask about combining medication with therapy.
- Make sure your mental health provider and OB are communicating.
If you’re thinking about starting medication, sertraline is the most studied and safest choice. Start low, go slow. Most women do well with doses between 50-100 mg per day.
And remember: you’re not choosing between a healthy baby and a healthy mom. You’re choosing the best way to have both.
Are antidepressants safe during pregnancy?
Yes, for most women, the benefits of taking antidepressants like sertraline or citalopram during pregnancy outweigh the risks. Large studies involving millions of births show no increased risk of birth defects or long-term developmental problems when compared to women with depression who don’t take medication. The key is choosing the right drug-avoid paroxetine-and working with your doctor to use the lowest effective dose.
Can antidepressants cause birth defects?
Early studies suggested a small link, but those didn’t account for the underlying depression. When researchers compared women with depression who took SSRIs to those who didn’t, the risk of birth defects disappeared. The exception is paroxetine, which is linked to a higher risk of heart defects. For this reason, doctors recommend switching away from paroxetine before or early in pregnancy.
What is neonatal adaptation syndrome?
It’s a temporary set of symptoms some newborns experience after being exposed to SSRIs in the womb. Signs include jitteriness, mild breathing trouble, or trouble feeding. These usually last only a few days to two weeks and don’t cause long-term harm. About 30% of exposed babies show some symptoms, but none require intensive treatment. Doctors monitor babies closely after birth and provide support as needed.
Should I stop my antidepressant if I find out I’m pregnant?
No. Stopping suddenly increases your risk of relapse by more than 60%. Depression during pregnancy raises the risk of preterm birth, low birth weight, and even maternal suicide. Instead of stopping, talk to your doctor about adjusting your dose or switching to a safer medication like sertraline. Never stop on your own.
Is therapy enough instead of medication?
For mild to moderate depression, cognitive behavioral therapy (CBT) can be as effective as medication. But for moderate to severe depression, therapy alone often isn’t enough. Many women benefit from combining both. If you’re trying therapy, make sure you have a backup plan. If your symptoms don’t improve in 4-6 weeks, medication may be necessary for your safety and your baby’s.
What’s the safest antidepressant during pregnancy?
Sertraline (Zoloft) is the most recommended. It has the most safety data, the lowest risk of side effects, and is least likely to cause complications like PPHN or neonatal adaptation syndrome. Citalopram and escitalopram are also good options. Fluoxetine is effective but carries a slightly higher risk of PPHN, so it’s often used only if other SSRIs haven’t worked.
Do antidepressants affect my baby’s brain development?
No. Long-term studies, including one tracking over 44,000 children in Norway up to age 5, found no differences in cognitive development, language skills, or behavior between children exposed to SSRIs in pregnancy and those who weren’t. The biggest risk to brain development comes from untreated maternal depression-not from the medication.
Webster Bull
December 12, 2025 AT 13:21Depression ain't a choice. Not taking meds? That's playing Russian roulette with your kid's future and your own life. The data's clear - staying stable is the only safe move.
Lauren Scrima
December 13, 2025 AT 04:50Oh, so now we're blaming moms for not being 'strong enough' to suffer silently? 😏
Lara Tobin
December 13, 2025 AT 08:40I was on sertraline through both pregnancies. My kids are 8 and 11 now - brilliant, happy, thriving. No developmental issues. Just a mom who got the help she needed. ❤️
Jamie Clark
December 15, 2025 AT 00:19That FDA panel was bought off by Big Pharma. You think they'd care about maternal suicide if it wasn't for profit? Wake up. This isn't science - it's a marketing campaign dressed in lab coats.
Keasha Trawick
December 15, 2025 AT 23:15Let’s be real - we’re talking about a neurochemical recalibration during a hyper-estrogenic, cortisol-drenched physiological state. SSRIs modulate 5-HT1A/2C receptor dynamics in utero, but the confounding variable is maternal HPA axis dysregulation - which, FYI, independently correlates with altered fetal neurogenesis. So yeah, the ‘risk’ is statistically noise when you account for the actual pathology.
Alvin Montanez
December 16, 2025 AT 12:55People don’t realize how dangerous this is. You think you’re being ‘natural’ by refusing meds? You’re not being brave - you’re being reckless. Depression doesn’t care if you’re ‘spiritual’ or ‘holistic.’ It doesn’t care if you drink chamomile tea and do yoga. It kills. It kills mothers. It kills babies. And then the internet clowns say ‘just meditate.’ You know what? I’ve sat in the ER with a woman who tried to end it all because she thought she ‘shouldn’t take pills.’ Don’t be that person. Get help. Now.
I’ve seen it. I’ve lived it. I’ve lost friends. This isn’t a debate. It’s a public health emergency wrapped in ignorance.
Jade Hovet
December 18, 2025 AT 09:42Thank you for this!! 🙏 I was terrified to tell my OB I was on Zoloft… but now I’m 32 weeks and my baby is kicking like a soccer champ 😊💖
nithin Kuntumadugu
December 19, 2025 AT 12:52Who funds these 'studies'? Big Pharma. They want you hooked. The real danger? The system that tells you your pain is a chemical imbalance so they can sell you pills. Your soul isn't broken - it's being exploited.
Try fasting. Try sunbathing. Try talking to your ancestors. Not a pill.
Rawlson King
December 19, 2025 AT 19:37So let me get this straight - you'd rather risk preterm birth, low birth weight, and maternal suicide because you're scared of a pill? This isn't bravery. It's ignorance dressed up as virtue.
John Fred
December 20, 2025 AT 16:18SSRIs + CBT = gold standard. Period. My wife did it - 75mg sertraline + weekly therapy. Baby delivered at 39w, Apgar 9/10. Mom? Still here. Still thriving. No regrets. 🤝
Harriet Wollaston
December 21, 2025 AT 18:13My sister had postpartum depression after her first and swore she’d never take meds again. She got pregnant again, hid it, and spiraled. Ended up in the psych ward. Don’t be like her. Ask for help. You deserve to feel okay.
sharon soila
December 21, 2025 AT 23:56It is imperative that expectant mothers receive evidence-based, multidisciplinary care. The conflation of anecdotal fear with clinical reality is both dangerous and unscientific. Pharmacological intervention, when appropriately monitored, is not only acceptable - it is ethically mandated in cases of moderate to severe depressive disorder.
nina nakamura
December 23, 2025 AT 07:11Everyone’s just ignoring the fact that SSRIs cross the placenta. No long-term studies beyond age 5? That’s not safety. That’s laziness. And now you’re telling women to take it anyway? You’re not a doctor. You’re a cheerleader for pharmaceuticals.