When you’re managing multiple medications, a simple mistake can lead to serious problems-like dangerous drug interactions, side effects you didn’t know about, or pills you’re taking that you no longer need. Telehealth medication reviews are designed to catch these issues before they hurt you. But unlike walking into a pharmacy or doctor’s office, this process happens over video. That means you need to be ready. You can’t just show up and hope for the best. If you don’t prepare, you might miss the chance to fix something that could keep you safe.
What Exactly Is a Telehealth Medication Review?
A telehealth medication review is a virtual meeting with a pharmacist or doctor who checks all the medicines you’re taking-prescription, over-the-counter, vitamins, supplements-and makes sure they’re working together safely. It’s not just a quick chat. It’s a full audit of your用药 history, your health conditions, and how you’re actually taking your pills. These reviews became widely used after 2020, when in-person visits dropped and health systems needed safer ways to manage chronic conditions like high blood pressure, diabetes, and depression. Today, 78% of U.S. healthcare systems offer them, and they’ve been shown to cut adverse drug events by nearly 35% in older adults.
The process usually starts with your doctor deciding you need one. Then, you’re connected with an accredited pharmacist who uses clinical tools to analyze your meds against your medical records, lab results, and pharmacy data. They look for duplicates, missing doses, interactions, and drugs that are no longer needed. The goal? Reduce hospital visits, prevent side effects, and make sure you’re not wasting money on pills you don’t need.
How to Prepare Before Your Appointment
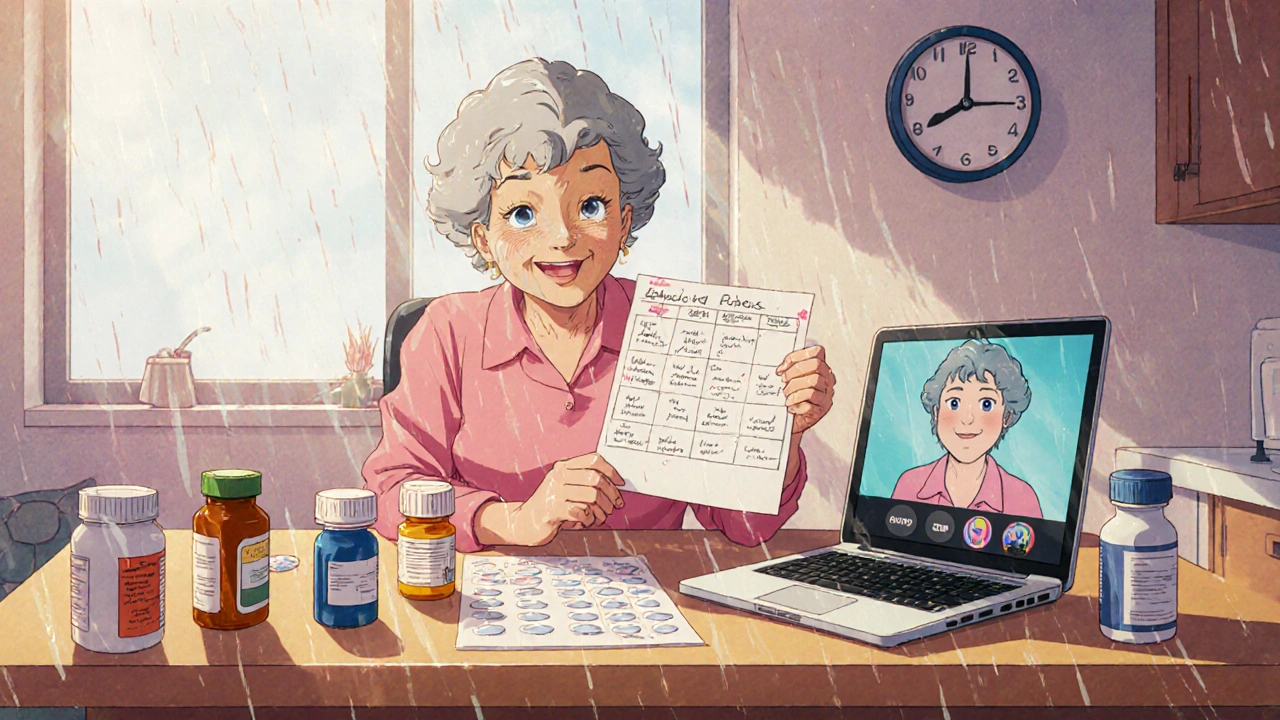
Preparation is what separates a helpful review from a frustrating one. Most people show up with a vague idea of what they take-and that’s not enough. Here’s what you need to do before your video call:
- Gather every medication you’re taking. This includes prescriptions, OTC painkillers, herbal supplements, vitamins, and even eye drops or patches. Don’t rely on memory. Pull out the bottles and lay them all on a table. A 2023 study found that patients who displayed their actual pills during the review had 37.4% more accurate assessments.
- Write down your dosing schedule. Note what you take, when, and how often. If you sometimes forget or skip doses, write that down too. Pharmacists need to know your real habits, not just what’s on the label.
- Bring your medical history. List any recent hospital stays, surgeries, or new diagnoses. Even small changes-like starting physical therapy or being diagnosed with kidney disease-can change which meds are safe for you.
- Test your tech ahead of time. Make sure your camera works, your internet is stable (at least 1.5 Mbps upload/download), and you know how to join the video call. Platforms like Doxy.me or Zoom for Healthcare are common. If you’re not tech-savvy, ask a family member to help you set up the day before.
- Write down your top concerns. What’s bothering you? Dizziness? Trouble sleeping? Upset stomach? Don’t wait for the pharmacist to ask. Lead with what matters to you.
If you’re over 65 or live in a rural area, you’re more likely to benefit from this service. But if you’ve never used video calls for health before, you’re not alone. A 2024 survey found that 68.2% of seniors felt more confident after getting a 10-minute tech tutorial before their appointment.
What to Ask During Your Review
You’re not just there to listen. You’re there to get answers. The pharmacist is trained to spot problems-but they won’t know what’s wrong unless you speak up. Here are the five most important questions to ask:
- “How will you make sure my medication list matches what my pharmacy and doctor have on file?” About 43% of medication errors come from mismatched records. If your pharmacist doesn’t cross-check your list with your pharmacy’s system, the review is incomplete.
- “Are any of these drugs no longer necessary?” Many people keep taking pills long after they’re needed-especially after surgery or hospital stays. One study found that 28% of older adults were still on antibiotics or painkillers they didn’t need six months after discharge.
- “What side effects should I watch for, and what should I do if I notice them?” Some side effects are mild. Others mean you need to stop the drug immediately. Get clear instructions. Don’t just be told “call your doctor.” Ask: “Should I call now? Go to urgent care? Or wait until tomorrow?”
- “How will you share your recommendations with my doctor?” Only 63% of telehealth services have a reliable system to send changes to your primary care provider. If your pharmacist doesn’t confirm this step, your changes might never happen.
- “How will you check in with me after this?” Virtual reviews have a blind spot: they can’t see if you’re swallowing your pills or if you’re having a reaction between visits. Ask if they’ll follow up by phone, text, or through a patient portal. Some programs use wearable monitors to track heart rate or blood pressure remotely-find out if that’s an option for you.
Don’t be afraid to ask for clarification. If they use a term like “polypharmacy” or “CYP450 interaction,” say, “Can you explain that in plain English?” You’re not being difficult-you’re protecting your health.
What This Service Can and Can’t Do
Telehealth medication reviews are powerful-but they’re not magic. They work best for stable, long-term conditions like high blood pressure, diabetes, thyroid issues, and depression. They’re excellent at catching duplicate prescriptions, eliminating expired drugs, and spotting dangerous combinations (like mixing blood thinners with NSAIDs).
But they have limits. If you have complex health issues-like dementia, severe mobility problems, or psychiatric conditions that need a full mental status exam-video alone isn’t enough. A 2021 study found that 17.3% of reviews for patients with multiple chronic illnesses were incomplete because the pharmacist couldn’t observe physical signs like swelling, skin rashes, or tremors. In these cases, you may still need an in-person visit.
Also, controlled substances like opioids (Schedule II) still require an initial in-person exam under DEA rules updated in January 2025. After that, follow-ups can be done virtually-but only if you’re under a special telemedicine registration. This doesn’t apply to most common medications like statins, metformin, or lisinopril.
Why This Matters for Your Safety
Medication errors are one of the leading causes of preventable harm in healthcare. In Australia, one in five hospital admissions for older adults is linked to medication problems. In the U.S., the cost of these errors is over $1,200 per patient each year. A well-run telehealth review can cut that risk dramatically.
Real people have had their lives changed by these reviews. One Reddit user reported that their virtual pharmacist caught three dangerous interactions their local pharmacy missed. Another found out they were taking two different versions of the same blood pressure pill-doubling their dose without knowing it.
But safety doesn’t come from the technology alone. It comes from your preparation, your questions, and your willingness to speak up. The system is built to help you. But you have to show up ready.
What Happens After the Review?
After your video call, the pharmacist will send a written summary to your doctor with recommendations: stop this drug, change the dose, add a new one, or schedule a follow-up. You should get a copy too-ask for it. If you don’t receive it within 48 hours, call your doctor’s office. Delays happen.
Your doctor doesn’t have to accept every suggestion, but they must respond to it. If they ignore a recommendation, ask why. You have the right to know.
Some systems now integrate with remote monitors-devices that track your blood pressure, heart rate, or oxygen levels and send data directly to your care team. If your provider offers this, sign up. It turns a one-time review into ongoing safety.
And if you feel something’s off after the review-new dizziness, confusion, rash, or nausea-don’t wait for your next appointment. Call your doctor or go to urgent care. Telehealth is a tool, not a replacement for your own instincts.
Do I need to be tech-savvy to do a telehealth medication review?
No. You just need a smartphone, tablet, or computer with a camera and internet. Most platforms are simple-just click a link. If you’re unsure, ask a family member to help you set up the day before. Many clinics offer free tech support calls for seniors. Don’t let fear of technology stop you.
Can I have a telehealth review if I take controlled substances like opioids or sleeping pills?
Yes-but only under certain rules. As of January 2025, the DEA requires an initial in-person visit for Schedule II drugs (like oxycodone or fentanyl). After that, follow-ups can be done via telehealth if your provider has a special registration. For Schedule III-V drugs (like hydrocodone or benzodiazepines), you can start and continue entirely online. Always confirm your provider’s DEA status before your appointment.
What if the video call freezes or cuts out during the review?
If the connection fails, ask to reschedule. Don’t continue if you can’t clearly see or be seen. You need to show your medications and be able to describe symptoms accurately. If this happens often, ask if they can switch to a phone call or if they offer a backup platform. A poor connection means a risky review.
How often should I get a telehealth medication review?
If you take three or more medications regularly, aim for one every 6 to 12 months. If you’ve recently been hospitalized, had surgery, or started a new drug, get one within 30 days. For older adults or those with chronic conditions, some clinics offer quarterly reviews. Ask your pharmacist what’s recommended for your situation.
Are telehealth medication reviews covered by insurance?
Yes, in most cases. Medicare and many private insurers cover comprehensive telehealth medication reviews under codes G2225 ($142.37) and G2226 ($78.92). You may still have a copay, but it’s usually similar to a regular doctor’s visit. Check with your insurer or ask the clinic before your appointment to confirm coverage.
Can I do a telehealth review if I don’t have a primary care doctor?
It’s harder, but possible. Some pharmacies and telehealth services offer standalone medication reviews. However, without a primary provider, it’s harder to ensure changes get implemented. If you don’t have a doctor, ask the pharmacist if they can connect you with a local clinic or community health center. Your safety depends on follow-through.
Next Steps for Better Medication Safety
After your review, take action. Keep a printed or digital list of your current meds and share it with every new provider. Use a pill organizer if you forget doses. Set phone reminders. Talk to your family about what you’re taking. And if something feels wrong-even after the review-trust your gut. You’re the expert on your own body. The pharmacist is there to help you see clearly. But you’re the one who has to act.
Shawn Sakura
November 22, 2025 AT 05:17Man, I was so scared to do this telehealth thing at first-thought I’d mess up the video call or forget what meds I’m on. But I just laid everything out on the table like they said, even my grandma’s fish oil capsules. Turned out I was doubling up on blood pressure pills. Pharmacist caught it. I cried. Not because I was upset-because I felt seen.
Don’t let fear stop you. Just show up with your bottles. You got this.
Swati Jain
November 23, 2025 AT 12:45Oh wow, so now we’re outsourcing our medication sanity to a Zoom pharmacist with a clipboard and a 1.5 Mbps connection? Brilliant. Next they’ll be diagnosing your depression via TikTok duet.
Let’s be real-this is cost-cutting disguised as ‘innovation.’ You think a screen can see if your hands are shaking? Or if you’re swallowing pills like candy? Please. They’re not replacing doctors-they’re replacing accountability.
Florian Moser
November 24, 2025 AT 08:24This is one of the most practical, well-structured guides I’ve ever read on telehealth med reviews. Every point is backed by data, and the preparation checklist is gold.
Especially the part about writing down your real dosing habits-not what’s on the bottle. That’s where most errors happen. People think they’re taking 10mg daily, but they’re taking 20mg on Tuesdays because ‘I felt bad that day.’ That’s not compliance-that’s chaos.
And yes, ask for the summary in writing. If they don’t send it, call. Persistence saves lives.
jim cerqua
November 25, 2025 AT 16:14THIS IS A SCAM. A FULL-ON CORPORATE CON JOB.
They want you to trust a stranger on a screen with your LIFE while your actual doctor is buried under 200 charts and a 30-second ‘review’ window.
I know a guy-his mom took 50 pills a day. Virtual review said ‘all good.’ Two weeks later, she was in the ER with kidney failure because they missed the NSAID + statin combo. The pharmacist? ‘Oh, I thought she meant she took them every other day.’
NO. NO. NO.
This isn’t safety. It’s liability laundering.
And don’t even get me started on the DEA loophole for opioids. They’re letting people get refills via FaceTime while real addicts are stuck in waiting rooms. This isn’t progress. It’s surrender.
Donald Frantz
November 27, 2025 AT 00:27Let’s cut through the fluff. The article says 78% of U.S. healthcare systems offer this. But how many actually do it well? How many pharmacists are overworked? How many reviews are 10 minutes long with a script? The stats look good, but real-world execution is a mess.
I’ve had three of these. Two were useless. One pharmacist didn’t even open my file until the last five minutes. I had to say, ‘I’m on metformin, lisinopril, and simvastatin-do you see them?’
Don’t assume the system works. Assume you’re the only one who cares enough to make it work.
Sammy Williams
November 28, 2025 AT 13:48Just did my first one last week. I was nervous as hell. My phone kept glitching. My cat jumped on the keyboard. I forgot to turn on the camera at first.
But the pharmacist was chill. She asked me to hold up each bottle. I showed her my fish oil, my melatonin, my leftover antibiotics from last year… and she said, ‘You’ve been taking this antibiotic for 18 months? For what?’
I didn’t even remember I was still on it. She told me to toss it. Felt like a weight lifted.
Do it. Even if you’re awkward. Even if your Wi-Fi sucks. Just do it.
Julia Strothers
November 30, 2025 AT 03:22Let me guess-this is all part of the Great Pharma Agenda. Telehealth reviews? Convenient for Big Pharma because now they don’t have to pay for in-person consultations. They can push more pills through the system with zero oversight.
And who’s reviewing the reviewers? Are these pharmacists even licensed? Or are they bots with a script? Did you know the DEA changed the rules in January 2025? That’s not a coincidence. That’s a cover-up.
They want you to think you’re safe. But you’re just another data point in their algorithm. Wake up.
And don’t even get me started on how they’re tracking your blood pressure through ‘wearables.’ That’s surveillance. That’s not healthcare.
Erika Sta. Maria
December 2, 2025 AT 01:36Wait-so you’re telling me that a pharmacist, who has never met me, can assess my ‘real habits’ just by me holding up bottles on video? That’s like judging a symphony by listening to a 10-second clip on a phone speaker.
And why are we accepting this as ‘progress’? We used to have doctors who came to our homes. We used to have community pharmacists who knew our names, our kids, our allergies. Now? We’re just another barcode in a system that doesn’t care if we live or die.
This isn’t medicine. It’s digital colonialism.
Also, I think the 35% reduction in adverse events is fabricated. Where’s the peer-reviewed study? I bet it was funded by a telehealth startup.
Nikhil Purohit
December 3, 2025 AT 04:40As someone who’s helped my mom through two of these, I can say: it’s not perfect, but it’s better than nothing.
My mom’s pharmacist found she was taking two different versions of the same blood pressure med-she didn’t even know they were the same drug. Saved her from a stroke.
Yes, tech glitches happen. Yes, some reviews are rushed. But if you prepare like they said-bottles, schedule, concerns-you’ll get value. Don’t let the perfect be the enemy of the good.
And if you’re in rural India like me? This is a lifeline. No one’s coming to your village. This is how you survive.
Debanjan Banerjee
December 3, 2025 AT 08:54Let’s be brutally honest: the system is broken, but this is the best tool we’ve got right now.
I’m a pharmacist in Bangalore. I’ve done 200+ telehealth reviews. Half the time, patients don’t know what they’re taking. Some think ‘vitamin C’ is the same as ‘ascorbic acid.’ Others take expired insulin because ‘it still looks fine.’
The checklist in this post? Non-negotiable. If you skip step one-laying out your bottles-you’re wasting everyone’s time.
And yes, the DEA rules are messy. But if you’re on a Schedule III drug like Xanax, you CAN do it online. Just confirm your provider’s DEA status. Don’t assume.
This isn’t magic. But it’s medicine with a little bit of hope.
Steve Harris
December 4, 2025 AT 14:38I’ve been on both sides of this-patient and caregiver. I’ve seen how powerful this can be, and I’ve seen how easily it can go wrong.
The key is not to treat it like a tech demo. Treat it like a life-saving conversation. Prepare like your life depends on it-because it does.
And if the pharmacist says something confusing? Ask again. Say, ‘Can you say that like I’m 10?’
They’ll respect you for it. Most of them are tired, overworked, and underpaid. They want you to succeed.
Just show up ready. That’s all they ask.
Michael Marrale
December 6, 2025 AT 01:39Hey, I just had to ask-do you think they’re using AI to generate the recommendations? Like, I saw a review where the pharmacist said, ‘Based on your age, gender, and meds, we recommend discontinuing…’
But then I checked the pharmacy’s website-same exact wording. Word for word.
Are we getting personalized care… or a template from ChatGPT?
Also, why do they always say ‘ask your doctor’? Who’s gonna fix it if they ignore the pharmacist? Nobody. That’s who.
I think we’re being fed a placebo. A digital placebo.
David vaughan
December 6, 2025 AT 13:31I’m not great with tech, but I did it anyway. I had my daughter help me set up the Zoom link. I printed out my meds list. I even wrote down why I was nervous: ‘I think I’m taking too many pills.’
She said, ‘You’re not taking enough of this one.’ I didn’t even know I was underdosing.
She said, ‘Your liver enzymes are elevated. You need to stop the ibuprofen.’
I cried.
It wasn’t perfect. The video froze once. But she stayed on the line until we fixed it.
Don’t let fear win. Just do it.
❤️
Cooper Long
December 8, 2025 AT 07:08The structural integrity of this guidance is commendable. The integration of empirical data with actionable protocol elevates the discourse beyond mere consumer advice into the realm of clinical best practice.
Particularly noteworthy is the emphasis on record reconciliation between pharmacy and provider systems-a systemic vulnerability historically underaddressed in outpatient care.
That said, the implicit assumption of digital equity remains a critical blind spot. For populations without reliable bandwidth or device access, this model may exacerbate disparities rather than mitigate them.
Telehealth is a tool-not a panacea.
Logan Romine
December 9, 2025 AT 05:09So we’ve turned medication safety into a Netflix documentary: ‘The Great Pill Audit: Season 1’.
Meanwhile, real people are dying because the system thinks ‘showing your bottles’ is enough to replace a physical exam.
And don’t even get me started on the ‘wearables’-now they’re tracking your heart rate so they can send you a push notification saying, ‘Hey, your BP is high. Maybe stop taking that pill you’ve been on for 10 years?’
😂
At this point, I just want someone to look me in the eye and say, ‘You’re okay.’ Not an algorithm. Not a pharmacist on Zoom. A human.
And if I can’t get that? I’m going back to the pharmacy counter. Even if I have to wait 4 hours.
💀