Every year, tens of thousands of people end up in the emergency room-not because of a fall, accident, or sudden illness-but because they took too much of the same medicine. Not because they meant to. Not because they were reckless. But because they didn’t realize they were taking it twice.
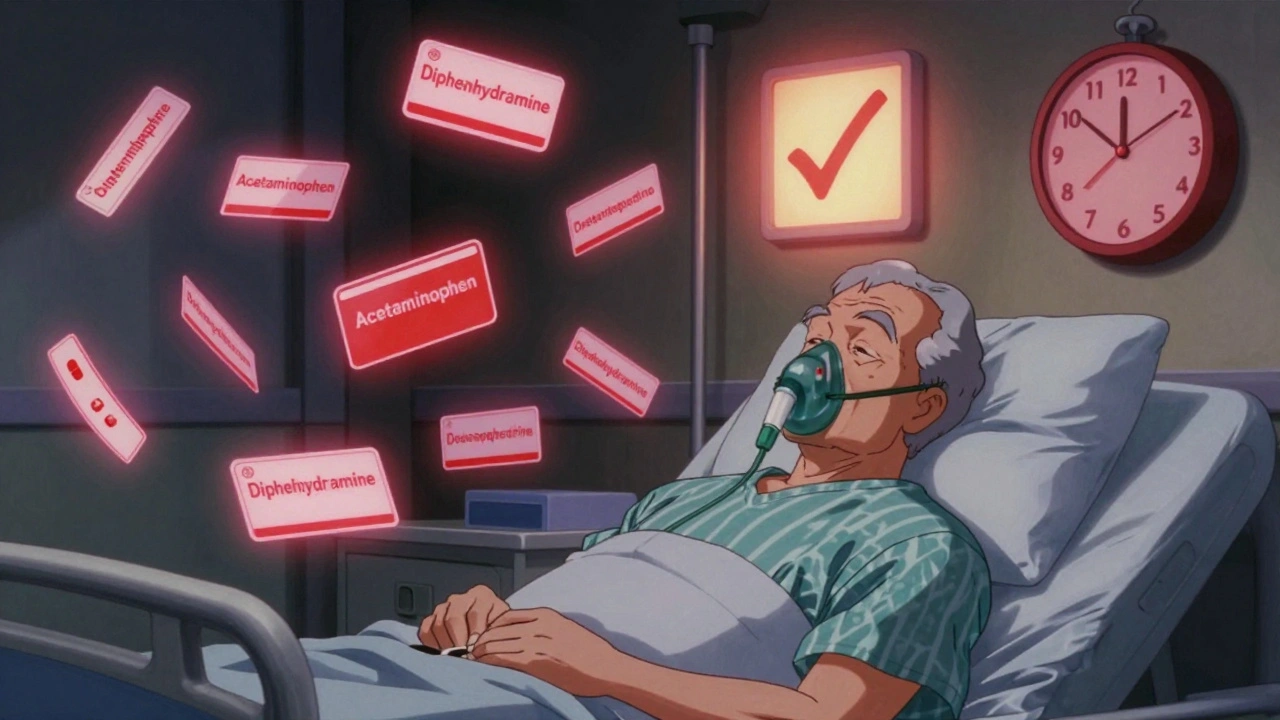
That’s the quiet danger of double ingredients. It’s when you take two or more medications that contain the same active ingredient. You might think you’re treating different symptoms: one pill for your headache, another for your cold, a third for your sleep. But if they all contain acetaminophen, diphenhydramine, or ibuprofen, you’re not getting better-you’re risking liver damage, extreme drowsiness, or even a stroke.
This isn’t rare. In the U.S., about 40% of adults over 65 take five or more medications regularly. And nearly one in three of them has accidentally taken a double ingredient at least once. The CDC says older adults account for 65% of hospitalizations caused by this exact mistake. But it’s not just seniors. Anyone taking prescription drugs and over-the-counter (OTC) medicines at the same time is at risk.
What Are Double Ingredients-and Why They’re Dangerous
Double ingredients happen when two or more drugs share the same active chemical. That chemical is what makes the medicine work. But if you take too much of it, your body can’t handle it.
The most common culprit? Acetaminophen. It’s in more than 600 different products-from painkillers like Vicodin and Percocet to cold medicines like Tylenol Cold, NyQuil, and store-brand versions. The NIH says 56,000 emergency room visits each year are due to accidental acetaminophen overdose. That’s more than 150 people a day.
Another big one is diphenhydramine. You’ll find it in allergy meds like Benadryl, sleep aids like Unisom, and even some cough syrups. It causes drowsiness. Take one, you might feel sleepy. Take two or three, and you could stop breathing. Dr. Ghada Ashkar from UCLA Health warns: “If you mix prescription sedatives with OTC antihistamines, the effects can be life-threatening.”
Then there’s pseudoephedrine, found in decongestants like Sudafed and many cold formulas. Taking multiple products with it can spike your blood pressure to dangerous levels. One Reddit user shared how taking three different cold medicines with pseudoephedrine landed him in the ER with severe hypertension.
And don’t forget NSAIDs like ibuprofen and naproxen. They’re in Advil, Aleve, and many arthritis and menstrual pain meds. Taking more than one at a time increases your risk of stomach bleeding, kidney damage, and heart problems.
The problem is hidden. You don’t see the danger on the front of the bottle. You see “Sinus Relief” or “Nighttime Sleep Aid.” You don’t see “Contains 500 mg acetaminophen” unless you read the tiny Drug Facts label.
Why This Keeps Happening
You might think, “I’m careful. I read labels.” But here’s the catch: most people don’t read the full label. A 2023 Government Accountability Office report found that 41% of patients still can’t identify shared ingredients from OTC Drug Facts labels-even after the FDA updated them in 2020 to make them clearer.
Prescription labels don’t help much either. A 2022 FDA review showed that 45% of prescription labels don’t mention if the drug shares ingredients with common OTC products.
And then there’s the multi-provider problem. If you see a cardiologist, a rheumatologist, and a pain specialist, each might prescribe something without knowing what the others have written. A 2021 study found that 82% of older adults who had double ingredient incidents visited multiple doctors in the past six months-and 67% said none of them ever asked about OTC meds.
Even worse, most people don’t tell their doctors about supplements, herbal remedies, or vitamins. The WHO says 68% of patients keep quiet about these. But some herbal products contain hidden ingredients-like kava or valerian-that can add to sedation or liver stress.
And if you fill prescriptions at different pharmacies? You’re flying blind. A 2021 JAMA study showed that using just one pharmacy cuts double ingredient errors by 63%. Why? Because that pharmacy’s system can see everything you’ve taken there and flag overlaps. Split your prescriptions across three stores? You lose that safety net.
The Real Numbers: Who’s Most at Risk
Let’s get specific:
- Adults 65+ are 65% of all hospitalizations from double ingredient errors.
- People taking five or more medications make up 82% of all double ingredient ER visits-even though they’re only 15% of the adult population.
- 73% of double ingredient cases involve cold and allergy medicines.
- 49% of incidents happen when people take multiple OTC products at once, thinking they’re “safe” because they’re not prescription.
- 32% of people on five or more meds have had a double ingredient experience.
And here’s the kicker: most of these cases are preventable. The American Academy of Family Physicians says 89% of double ingredient errors could be avoided with a simple, updated medication list.
How to Protect Yourself: 5 Action Steps
You don’t need a pharmacy degree to avoid this. You just need to change a few habits.
- Make a full medication list-every single thing you take. Not just prescriptions. Include OTC pills, vitamins, supplements, herbal teas, and even topical creams. Write down the name, dose, how often you take it, and why. Keep a copy in your wallet and one at home. Update it every time you start or stop something.
- Take this list to every doctor and pharmacist visit. Don’t wait for them to ask. Say: “Here’s everything I’m taking. Can you check for duplicates?” If you see multiple providers, bring the same list to each one. Ask: “Is this new medicine safe with what I’m already on?”
- Fill all prescriptions at one pharmacy. This is the single most effective step. Pharmacies have systems that check for interactions and duplicates. If you use multiple pharmacies, they can’t see what’s in your other bottles. One pharmacy = one clear picture.
- Read the Drug Facts label on every OTC product. Look for “Active Ingredients.” If you see the same name as one of your prescriptions, don’t take it. For example, if your painkiller has acetaminophen, don’t take NyQuil, DayQuil, or Excedrin. Use plain saline spray or a humidifier instead.
- Ask your pharmacist to review your meds once a year. Many pharmacies offer free Medication Therapy Management (MTM) services. In 87% of these reviews, pharmacists catch a potential double ingredient or interaction you didn’t know about.
What’s Being Done to Fix This
This isn’t just a personal problem-it’s a system-wide one. And change is happening.
The American Geriatrics Society updated its Beers Criteria in 2023 to list 15 high-risk double ingredient combinations, especially for older adults. The FDA launched a new labeling initiative in January 2024 that requires all OTC products to display active ingredients in a standardized, bold format. Full compliance is required by December 2025.
Electronic health records from Epic and Cerner now include automatic double ingredient checks. They flag matches between prescriptions and OTC meds-when the data is entered. But here’s the gap: only 43% of these systems track OTC use properly. So if you don’t tell your doctor about your cold medicine, the system won’t know.
Apple Health, starting with iOS 17 in 2023, now warns you if you try to add a new medication that contains the same active ingredient as one you’re already tracking. It’s not perfect, but it’s a start.
Medicare Part D plans now use the Pharmacy Quality Alliance’s Drug-Drug Interactions measure. Since 2021, it’s cut senior hospitalizations from double ingredient errors by 28%.
But technology alone won’t save you. Only you can make sure your list is complete, your pharmacy is consistent, and your doctors know everything you’re taking.
What to Do If You Think You’ve Taken Too Much
Symptoms of double ingredient overdose vary by ingredient:
- Acetaminophen: Nausea, vomiting, loss of appetite, pain in the upper right abdomen. Later: yellow skin or eyes, confusion, extreme fatigue.
- Diphenhydramine: Extreme drowsiness, blurred vision, dry mouth, trouble urinating, fast heartbeat, hallucinations.
- Pseudoephedrine: Severe headache, dizziness, rapid heartbeat, chest pain, high blood pressure.
- NSAIDs: Black or bloody stools, vomiting blood, stomach pain, reduced urination.
If you notice any of these and suspect you’ve taken too much of one ingredient, call Poison Control at 1-800-222-1222 or go to the ER. Don’t wait. Don’t hope it’ll pass. Acetaminophen overdose can cause liver failure within 72 hours-often with no warning until it’s too late.
Final Thought: Your List Is Your Shield
Medications save lives. But when they overlap, they can destroy them. The biggest myth is that “OTC means safe.” It doesn’t. The biggest mistake is thinking “my doctor knows what I’m taking.” They don’t-not unless you tell them.
Take five minutes today. Write down every pill, drop, patch, and supplement you use. Include the brand, the dose, and why you take it. Then take it to your next appointment. Ask: “Is there anything here that’s the same as something else?”
That one list could be the difference between healing and hospitalization.
Can I take two different cold medicines if one is for daytime and one is for nighttime?
No. Most daytime and nighttime cold medicines contain the same active ingredients-just in different doses. Daytime formulas often have pseudoephedrine and acetaminophen. Nighttime formulas add diphenhydramine. But you’re still getting acetaminophen twice. Taking both can lead to liver damage. Pick one formula and stick with it. If symptoms persist, talk to your pharmacist.
I take a prescription painkiller. Can I still use Advil or Tylenol for extra pain?
It depends. If your prescription painkiller already contains acetaminophen (like Vicodin or Percocet), do not take Tylenol. You’ll overdose. If it contains ibuprofen or naproxen, don’t take Advil or Aleve. If your prescription is just an opioid like oxycodone without any pain reliever, you can take acetaminophen or ibuprofen-but only after checking with your doctor or pharmacist. Never assume it’s safe.
Does my pharmacy automatically know what OTC medicines I’m taking?
No. Pharmacies only track what you buy at their store. If you buy Benadryl at Walmart and your prescriptions at CVS, your CVS pharmacist won’t know you’re taking it. That’s why you must tell them. Always bring your full list to the pharmacy-even if you’re just picking up one new pill.
I’m on blood pressure meds. Is it safe to take a decongestant for a stuffy nose?
Not usually. Decongestants like pseudoephedrine and phenylephrine can raise your blood pressure and interfere with your meds. Instead, try saline nasal spray, a humidifier, or a non-decongestant antihistamine like loratadine (Claritin). Always ask your pharmacist before taking anything for a cold if you have high blood pressure.
How often should I review my medications?
At least once a year-and anytime you start or stop a medicine, see a new doctor, or notice new side effects. Many people don’t realize they’re taking something until they have a problem. A yearly review with your pharmacist can catch hidden overlaps before they cause harm.

Katie Harrison
December 9, 2025 AT 13:25I used to take NyQuil and Advil together because I thought, 'It's just a cold and a headache'-until I ended up in the ER with liver enzymes through the roof. Never again. I keep a printed list in my wallet now. It’s annoying, but it’s saved my life.
Mona Schmidt
December 9, 2025 AT 17:59The FDA’s 2024 labeling update is a step forward, but it’s still insufficient. Many elderly patients, especially those with low vision or cognitive decline, cannot read small print-even if it’s bolded. There needs to be a mandatory audio-label option on all OTC packaging, linked via QR code. This isn’t just about awareness-it’s about accessibility.
Guylaine Lapointe
December 10, 2025 AT 19:44People are just lazy. If you can’t read a label, maybe you shouldn’t be taking meds. I don’t feel bad for folks who mix NyQuil with Tylenol-your ignorance is not my problem. I’ve seen too many people treat pharmacies like candy stores. Get your act together.
Chris Marel
December 12, 2025 AT 12:06In Nigeria, we don’t have the same access to pharmacists, but we do have community health workers who help elderly neighbors check their meds. Maybe we need more of that model everywhere-someone who sits with you, reads the tiny print, and asks, 'What else are you taking?' It’s not about blame-it’s about care.
Angela R. Cartes
December 13, 2025 AT 10:00OMG I just realized I’ve been taking DayQuil AND my prescription for migraines (which has acetaminophen) for months 😱 I’m deleting my cold meds right now. Thanks for the scare, OP. 🙏
Larry Lieberman
December 15, 2025 AT 08:54Just checked my meds-turns out my 'sleep aid' and my 'allergy pill' both have diphenhydramine. 🤯 I’ve been nodding off at my desk for months. Also, why does every cold medicine have the same 3 ingredients? It’s like they’re trying to kill us with convenience. 🤦♂️
Brianna Black
December 17, 2025 AT 06:44This is not merely a public health issue-it is a systemic failure of communication, education, and corporate transparency. The pharmaceutical industry profits from the confusion it creates. Why are active ingredients buried in fine print? Why are combination products marketed as 'comprehensive relief' when they are, in fact, chemical landmines? We must demand accountability-not just personal vigilance.
My mother, 78, takes eight prescriptions and six supplements. She trusts her doctors. She does not know that one of her supplements contains kava, which interacts with her blood thinner. No one asked. No one checked. This is negligence dressed as healthcare.
The solution is not a list. It is a mandatory, centralized, real-time medication registry-linked across all providers, pharmacies, and insurers-with automatic alerts for overlaps. Until then, we are all just playing Russian roulette with our livers.
And yes-I’ve taken my list to every appointment since reading this. I now carry a laminated copy. I am no longer passive. I am a patient advocate. And you should be too.
Shubham Mathur
December 18, 2025 AT 22:29