When you’re taking more than one medication, it’s not just about whether each drug works on its own - it’s about how they interact with each other. Two drugs might be perfectly safe alone, but together, they could cause dangerous side effects, reduce effectiveness, or even lead to hospitalization. The key to understanding these risks lies in two fundamental concepts: pharmacokinetic and pharmacodynamic interactions. These aren’t just textbook terms - they’re the difference between a medication working as intended and a serious health crisis.
What Pharmacokinetic Interactions Really Mean
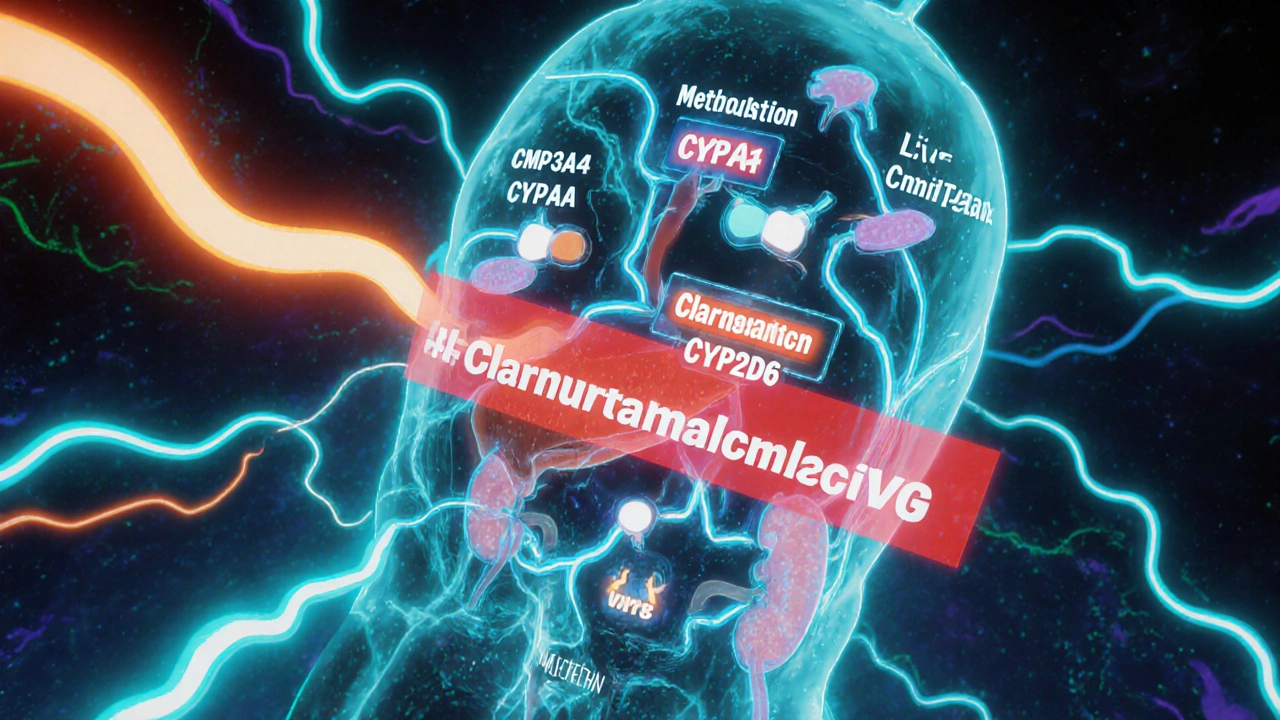
Pharmacokinetics is what the body does to the drug. Think of it like a delivery system: how a drug gets into your bloodstream, where it goes, how long it stays, and how it leaves your body. These processes - absorption, distribution, metabolism, and excretion (ADME) - are where pharmacokinetic interactions happen. One of the most common ways this goes wrong is through drug metabolism. Your liver uses enzymes, especially the CYP3A4, CYP2D6, and CYP2C9 families, to break down medications. If one drug blocks or speeds up these enzymes, it changes how much of another drug is active in your system. For example, clarithromycin (an antibiotic) is a strong CYP3A4 inhibitor. When taken with simvastatin (a cholesterol drug), it can cause simvastatin levels to spike by up to 10 times. That’s not a small change - it’s enough to trigger muscle damage, kidney failure, or even rhabdomyolysis. The FDA recommends cutting simvastatin’s dose to 10 mg or avoiding the combo entirely. Other examples:- Antacids like Tums can reduce absorption of antibiotics like ciprofloxacin by up to 90%, making them useless.
- Warfarin, a blood thinner, can be pushed off protein-binding sites by drugs like phenylbutazone, increasing its free concentration by 300% and raising bleeding risk.
- Probenecid, used for gout, blocks kidney excretion of penicillin, keeping it in your system longer - sometimes intentionally, to boost effectiveness.
What Pharmacodynamic Interactions Are All About
Pharmacodynamics is what the drug does to your body. It’s about the effect at the target - whether that’s a receptor, enzyme, or nerve pathway. Pharmacodynamic interactions happen when two drugs affect the same system, even if their levels in the blood stay normal. There are three main types:- Synergistic: The combined effect is stronger than the sum of each drug. Sildenafil (Viagra) and nitroglycerin together can cause a dangerous drop in blood pressure - so much so that this combo is strictly contraindicated.
- Additive: Effects simply add up. Taking aspirin with warfarin increases bleeding risk because both thin the blood, just in different ways.
- Antagonistic: One drug blocks the other. Naloxone reverses opioid overdoses by kicking opioids off their receptors. Beta-blockers can cancel out the effects of albuterol in asthma patients.
Why the Difference Matters for Treatment
Knowing whether an interaction is pharmacokinetic or pharmacodynamic changes how you manage it. If it’s pharmacokinetic - say, a drug is boosting another’s concentration - you can often fix it by lowering the dose. That’s why guidelines say to reduce simvastatin when paired with clarithromycin. You’re not stopping the combo - you’re adjusting for the altered delivery. But if it’s pharmacodynamic - like combining two drugs that both lower blood pressure - you can’t just tweak the dose. The effect isn’t about concentration; it’s about the body’s response. In these cases, avoidance is the only safe option. You can’t safely lower the dose of both drugs and still treat the conditions. This distinction is why pharmacists now use tools like the Flockhart Table and electronic health record alerts. Epic’s 2023 system flags over 1,200 high-risk pharmacokinetic interactions and nearly 1,000 pharmacodynamic ones. But alerts aren’t perfect. Many clinicians still miss subtle PD interactions because they’re looking for lab changes, not clinical outcomes.
Who’s at Highest Risk?
Older adults are the most vulnerable. About 15% of people over 65 take five or more medications daily, according to CDC data. Each additional drug multiplies interaction risk. Polypharmacy isn’t just about quantity - it’s about complexity. Drugs with narrow therapeutic indexes - where the difference between a therapeutic dose and a toxic one is tiny - are especially dangerous. Warfarin, digoxin, lithium, and phenytoin fall into this category. Over 68% of serious interactions with these drugs are pharmacokinetic. CNS drugs are another hotspot. Antidepressants, antipsychotics, and opioids often interact pharmacodynamically. Mixing an SSRI with tramadol, for example, can trigger serotonin syndrome - even if both drugs are prescribed legally. Even newer drugs aren’t safe. Immune checkpoint inhibitors used in cancer therapy can have dangerous pharmacodynamic interactions with immunosuppressants, increasing infection or autoimmune risk. The EMA flagged these in 2023 as a growing concern.How to Stay Safe
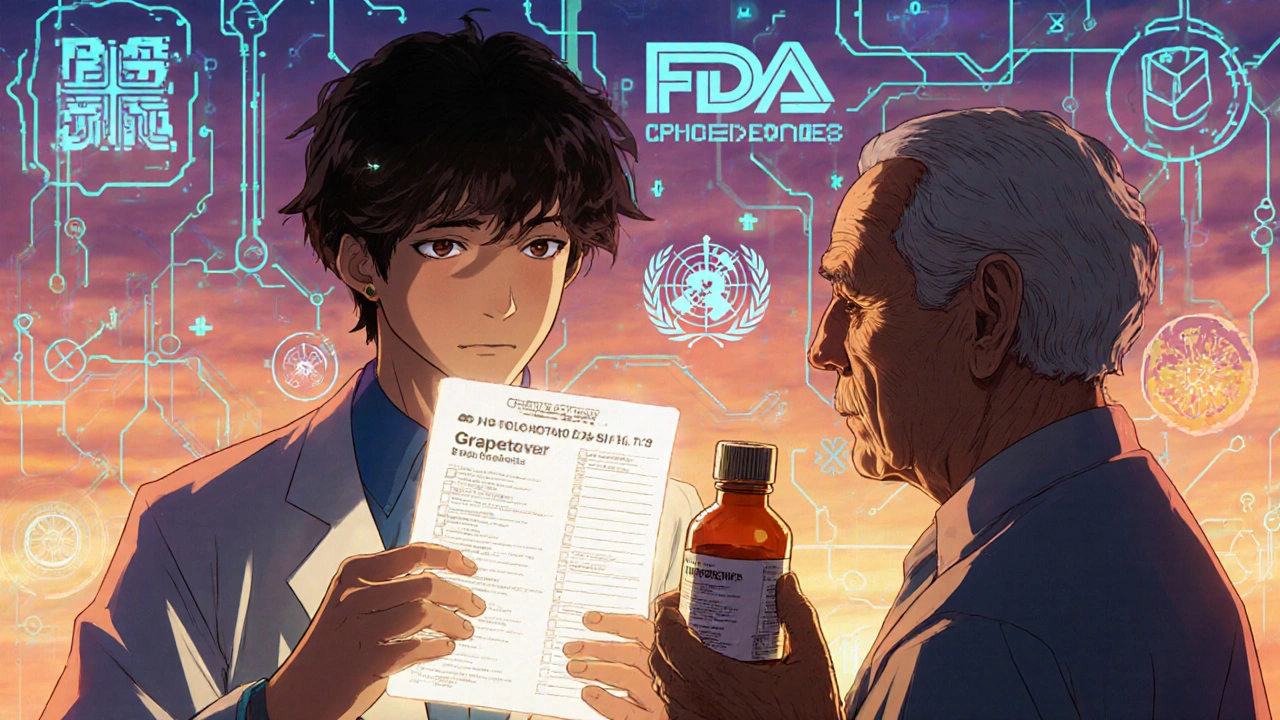
You don’t need to be a doctor to protect yourself. Here’s what works:- Know your meds. Keep a list of everything you take - including OTC drugs, supplements, and herbs. St. John’s wort, for example, induces CYP3A4 and can reduce effectiveness of birth control, cyclosporine, and many antidepressants.
- Ask your pharmacist. They’re trained to spot interactions. Studies show pharmacist-led reviews reduce adverse events by 42%.
- Watch for new symptoms. If you start a new drug and feel dizzy, nauseous, unusually tired, or have bleeding or swelling, don’t wait. These could be interaction signs.
- Don’t assume natural means safe. Grapefruit juice blocks CYP3A4. It can double levels of statins, calcium channel blockers, and even some anxiety meds.
- Use one pharmacy. It helps them track everything you’re on and catch red flags.
The Future of Drug Interaction Safety
Science is catching up. The FDA now requires testing against 11 CYP enzymes and 8 transporters - up from just 7 in 2017. Pharmacogenomics is making it possible to predict who’s at risk based on their genes. CPIC’s 2023 guidelines now cover 32 gene-drug pairs that change interaction risk. AI models are also stepping in. A 2023 study in Nature Medicine showed machine learning could predict pharmacodynamic interactions with 89% accuracy - better than traditional methods. Real-world data from the FDA’s Sentinel Initiative has already identified 17 new risky combos, like SGLT2 inhibitors (for diabetes) with loop diuretics, which increase dehydration risk by over two-fold. The World Health Organization estimates that better understanding of these interactions could prevent 1.3 million adverse events globally by 2030 - saving $28 billion in healthcare costs.Bottom Line
Pharmacokinetic interactions change how much drug is in your system. Pharmacodynamic interactions change how your body responds to it. One can often be managed with a dose change. The other usually requires avoiding the combo altogether. If you’re on multiple medications, especially if you’re over 65 or have chronic conditions, don’t assume your drugs are safe just because they were prescribed. Ask: Is this interaction about concentration - or about effect? That one question could save your life.What’s the difference between pharmacokinetic and pharmacodynamic drug interactions?
Pharmacokinetic interactions affect how your body processes a drug - things like absorption, metabolism, and excretion. They change the drug’s concentration in your blood. Pharmacodynamic interactions affect how the drug works in your body - like when two drugs target the same receptor or system, making their effects stronger, weaker, or dangerous. One is about amount; the other is about effect.
Can pharmacokinetic interactions be fixed with a dose change?
Yes, often they can. If one drug increases the level of another - like clarithromycin raising simvastatin levels - lowering the dose of the affected drug can reduce risk. That’s why guidelines recommend reducing simvastatin to 10 mg when taken with certain antibiotics. But if the interaction involves a drug with a narrow therapeutic window, like warfarin, close monitoring is still essential.
Why are pharmacodynamic interactions harder to detect?
Because they don’t change drug levels in your blood. You can have perfectly normal lab results and still experience a dangerous reaction - like serotonin syndrome from mixing SSRIs and tramadol. These interactions depend on how your body’s systems respond, not on how much drug is present. That’s why symptoms like dizziness, confusion, or low blood pressure might appear suddenly, even with no change in dosage.
Which drugs are most likely to cause dangerous interactions?
Drugs with narrow therapeutic indexes - like warfarin, digoxin, lithium, and phenytoin - are high-risk for pharmacokinetic interactions. For pharmacodynamic interactions, CNS drugs (antidepressants, opioids, antipsychotics), anticoagulants, and antihypertensives are the biggest concerns. Even common OTC drugs like ibuprofen or St. John’s wort can cause serious interactions.
Should I stop taking my meds if I’m worried about interactions?
Never stop a prescribed medication without talking to your doctor or pharmacist. Many interactions can be managed safely - with dose changes, timing adjustments, or switching to an alternative. Stopping suddenly can be more dangerous than the interaction itself. Always bring your full medication list to every appointment, including supplements and herbal products.
Iska Ede
November 17, 2025 AT 21:39So let me get this straight - we’re telling people to avoid grapefruit juice because it turns their statin into a grenade, but it’s totally fine to chug energy drinks with their blood thinner? 😒 I’m just saying, if your meds come with a warning label that reads like a horror movie plot, maybe the system’s broken.
Also, St. John’s wort is basically the keto diet of herbal supplements - everyone swears by it until someone ends up in the ER.
And don’t even get me started on ‘natural’ = safe. My grandma took ‘natural’ turmeric pills and ended up bleeding out after her knee surgery. Natural doesn’t mean ‘not a drug.’ It just means ‘not regulated.’
Gabriella Jayne Bosticco
November 18, 2025 AT 08:16I’ve been on five meds for years and honestly, I just hand my list to the pharmacist every time I refill. They’re the real MVPs.
One time they caught that my OTC sleep aid was canceling out my blood pressure med - I had no idea. They switched me to a different one and my numbers went from ‘concerning’ to ‘perfect.’
Don’t be shy about asking. Pharmacists don’t get paid enough to do this, but they still do it anyway. Seriously, thank you to every pharmacist who doesn’t roll their eyes when you show up with a grocery bag full of bottles.
Bailey Sheppard
November 18, 2025 AT 12:18This is one of those posts that makes you realize how little we’re taught about our own bodies. I mean, I’ve been on antidepressants for a decade and never knew that mixing them with tramadol could cause serotonin syndrome - not even my doctor mentioned it.
It’s not just about the drugs, it’s about the system. We treat prescriptions like they’re magic bullets, not complex chemical interactions.
Maybe we need a mandatory ‘Medication 101’ class in high school. Not just ‘don’t do drugs,’ but ‘here’s how your body actually works with what you put in it.’
Also, one pharmacy only. Do it. It’s the easiest life hack you’ll ever find.
Louie Amour
November 19, 2025 AT 02:53Let’s be honest - most of these ‘interactions’ are just lazy prescribing. If you’re giving someone five drugs with overlapping CYP pathways, you’re not a doctor, you’re a carnival barker with a prescription pad.
And don’t get me started on the FDA’s ‘11 CYP enzymes’ checklist. That’s not science - that’s bureaucratic box-ticking. Real pharmacology isn’t about memorizing enzyme names, it’s about understanding physiology.
Also, AI predicting interactions at 89% accuracy? That’s not progress. That’s just admitting we’ve been flying blind for 50 years. Congrats, medicine - you’re finally catching up to the 1990s.
Kristina Williams
November 20, 2025 AT 20:35Did you know the government is secretly using these drug interactions to control the population? They want us to be confused and dependent. That’s why they don’t tell you about the real dangers - like how grapefruit juice is actually a mind-control agent disguised as fruit.
Also, the CDC says 15% of seniors take 5+ meds? That’s not an accident. That’s a rollout. They’re testing the ‘pharmaceutical dependency’ theory on old people first. Next stop: your kids.
And why do you think they call it ‘therapeutic drug monitoring’? It’s not monitoring - it’s surveillance. They’re watching your blood levels to see if you’re resisting.
Shilpi Tiwari
November 22, 2025 AT 16:42From a pharmacogenomics standpoint, the CYP2D6 ultrarapid metabolizer phenotype is a critical confounder in SSRI-narcotic co-administration scenarios - particularly in populations with high allelic frequency of *1/*1xN or *2/*2xN duplications, which are prevalent in South Asian cohorts.
Moreover, the pharmacodynamic synergy between SGLT2 inhibitors and loop diuretics is mediated via NCC cotransporter downregulation and subsequent volume depletion, which amplifies the risk of acute kidney injury in elderly patients with reduced GFR.
It’s not enough to just know the interaction - you need to model the kinetic-dynamic interface using population PK/PD frameworks. Otherwise, you’re just guessing.
Christine Eslinger
November 24, 2025 AT 05:50I’ve spent years working in mental health, and I’ve seen too many people suffer because their doctor didn’t understand the difference between PK and PD interactions.
One patient was on sertraline and started taking a new OTC cold med - no one told her it contained dextromethorphan. She ended up in the hospital with serotonin syndrome. Her blood levels were normal. Her brain wasn’t.
It’s not about being scared of meds. It’s about being informed. Your body isn’t a black box - it’s a conversation. And every drug you take is one more voice in that conversation.
Don’t be afraid to ask, ‘Is this about how much is in my blood… or how my body is responding?’ That question alone can save you.
Also, always bring your supplements to your appointments. I’ve lost count of how many times ‘just a little turmeric’ turned into a bleeding emergency.
Denny Sucipto
November 25, 2025 AT 07:38Man, I used to think if it was in a pill, it was fine. Then my buddy took that ‘miracle’ weight loss tea with his heart med and ended up in the ER with his heart doing the cha-cha.
Turns out the tea had this ‘natural’ stimulant that acted like a speedball with his beta-blocker. He didn’t even know what was in it.
So now I tell everyone: if you’re taking more than three things, make a list. Write it down. Take it to the pharmacy. Don’t trust your memory. Don’t trust the label. Don’t trust ‘natural.’
And if you’re feeling weird after starting something new? Don’t wait. Call someone. It’s not panic - it’s smart.
Also, grapefruit juice? Just say no. It’s not worth it.
Holly Powell
November 26, 2025 AT 12:51How is this still a conversation? We have pharmacogenomic databases, AI-driven interaction predictors, and real-time EHR alerts - yet we’re still relying on patients to ‘ask their pharmacist’ like it’s 1987?
And why is the FDA only requiring testing against 11 CYP enzymes? That’s laughable. There are over 50 known transporters and phase II enzymes that aren’t even on the radar.
Most clinicians still think ‘interaction’ means ‘liver enzyme’ - they don’t understand receptor-level pharmacodynamics. That’s not negligence - it’s institutional incompetence.
And don’t get me started on ‘natural’ supplements. They’re unregulated, untested, and often contaminated with synthetic analogs. It’s a minefield disguised as wellness.
Emanuel Jalba
November 27, 2025 AT 00:53THIS IS A TRAP. 😱
They don’t want you to know this - but EVERY SINGLE DRUG INTERACTION is designed to keep you hooked. The pharmaceutical companies know that if you take one drug, you’ll need another to fix the side effect… then another to fix THAT one.
That’s why they don’t warn you about grapefruit juice - they WANT you to need more pills.
And the FDA? They’re in on it. They approved every single one. Why? Because they get paid by Big Pharma. 😤
STOP TAKING MEDS. GO NATURAL. EAT CUCUMBERS. 🥒
My cousin stopped all meds and now she’s ‘healed’ - no more diabetes, no more high blood pressure. Just cucumbers and prayer. 🙏
They don’t want you to know the truth. But now YOU DO. 💪
Heidi R
November 27, 2025 AT 05:41So you’re telling me I should trust a pharmacist who works at CVS? 😏
They’re just reading from a screen. They don’t know my history. They don’t care. And if you ask a question? They’ll hand you a pamphlet and say ‘ask your doctor.’
Meanwhile, your doctor’s in and out in 7 minutes. They’re not checking your supplements. They’re not reading the FDA’s 1,200 alerts. They’re billing.
Don’t be naive. This system is designed to keep you sick and paying.
Just stop taking everything. You’ll be fine.