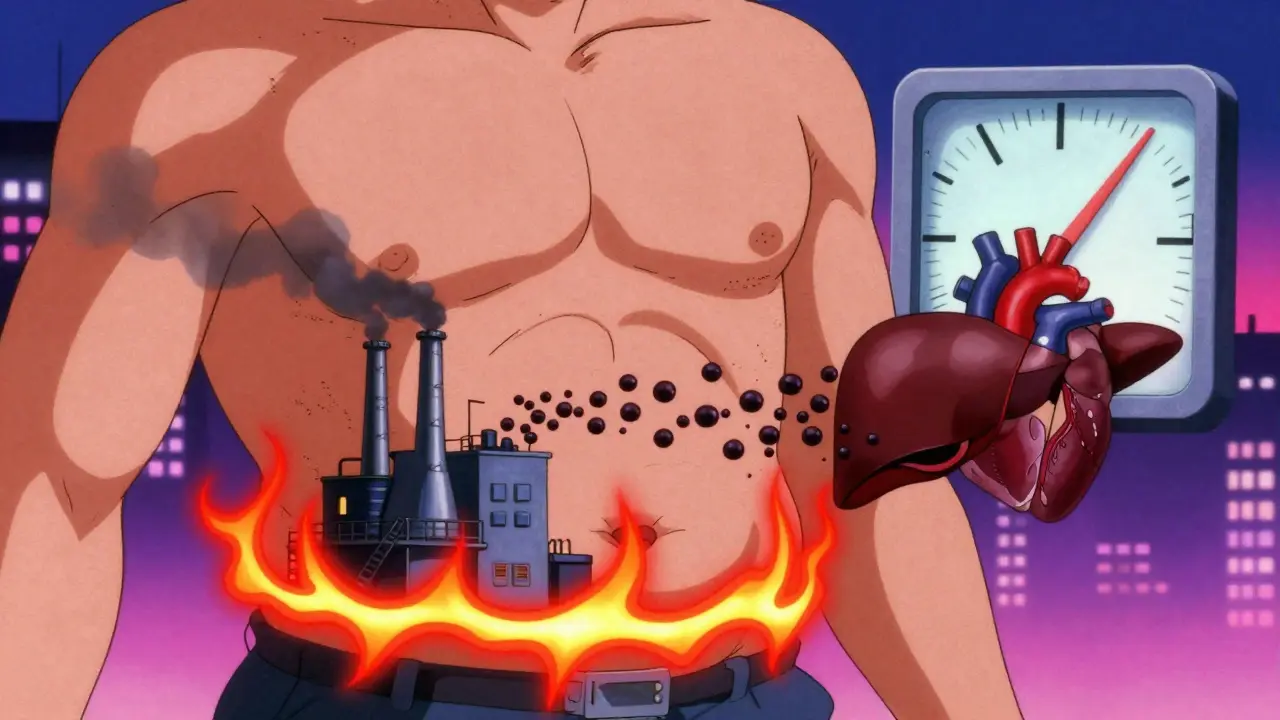
Think of your body like a car. If the engine is running hot, the oil is dirty, and the fuel system is clogged, it doesn’t matter how new the tires are - something’s wrong underneath. Metabolic syndrome is that same kind of warning light, but for your metabolism. It’s not one disease. It’s a cluster of three key problems: too much belly fat, high triglycerides, and blood sugar that won’t stay in check. And together, they crank up your risk for heart disease, stroke, and type 2 diabetes - fast.
What Exactly Is Metabolic Syndrome?
Metabolic syndrome isn’t a diagnosis you get from a single blood test. It’s a pattern. If you have at least three of these five signs, you have it:
- Waist size over 40 inches for men, or 35 inches for women
- Triglycerides at 150 mg/dL or higher
- HDL (good cholesterol) below 40 mg/dL for men, or 50 mg/dL for women
- Blood pressure at 130/85 mm Hg or higher
- Fasting blood sugar at 100 mg/dL or higher
The National Heart, Lung, and Blood Institute says about 35% of U.S. adults have this mix. In Australia, the numbers are rising too - especially among people over 50. But here’s the thing: you don’t need to be overweight to have it. Some people with normal BMI still carry fat deep inside their abdomen, and that’s the real danger.
Why Waist Size Matters More Than You Think
It’s not just about how you look in the mirror. Belly fat - the kind that hugs your organs - is metabolically active. It’s not just storage. It’s a factory. It pumps out inflammatory chemicals that mess with how your body uses insulin. That’s the first domino.
Research from the Circulation journal shows every extra 4 inches around your waist raises your heart disease risk by 10%, even if your weight stays the same. That’s why doctors now measure waist size - not just BMI. A man with a 38-inch waist and normal weight has a higher risk than someone with a 32-inch waist who weighs more.
And it’s not just Western populations. South Asian, Middle Eastern, and some Indigenous groups develop metabolic problems at much smaller waist sizes - sometimes as low as 31.5 inches for women. That’s why global guidelines now adjust thresholds by ethnicity. If you’re from these backgrounds, don’t wait for a big waist to act.
Triglycerides: The Silent Red Flag
Triglycerides are a type of fat in your blood. They come from the food you eat, especially sugar and alcohol. But when your body can’t use insulin properly, your liver starts making too many of them. That’s why high triglycerides and high blood sugar often show up together.
A level of 150 mg/dL is the minimum to count toward metabolic syndrome. But if you’re above 200 mg/dL, your risk for heart attack or stroke jumps even without other factors. The American Heart Association calls this a high-risk zone. And it’s not just about diet. Insulin resistance forces your liver to churn out more triglycerides as VLDL particles - the kind that stick to artery walls.
Here’s what most people don’t realize: cutting out soda, candy, and white bread can slash triglycerides faster than medication. One study showed a 30% drop in just 3 weeks with simple dietary changes.

Glucose Control: The Body’s Alarm System
Fasting blood sugar at 100 mg/dL or higher means your body is struggling to handle glucose. This isn’t diabetes yet - it’s prediabetes. But it’s your body screaming for help.
The Diabetes Prevention Program tracked over 3,000 people with prediabetes. Those who lost 5-7% of their body weight and walked 150 minutes a week cut their diabetes risk by 58%. That’s more effective than metformin, the common diabetes drug.
And here’s the twist: high triglycerides make insulin resistance worse. Fat molecules build up in muscle cells and block insulin from doing its job. So your pancreas pumps out more insulin to compensate. Eventually, it burns out. That’s when blood sugar climbs for good.
The Vicious Cycle: Fat, Fat, and More Fat
This isn’t three separate problems. It’s one broken system.
Abdominal fat → releases chemicals → causes insulin resistance → liver makes more triglycerides → muscles can’t take up glucose → blood sugar rises → more fat storage → worse insulin resistance.
It’s a loop. And it feeds on itself. That’s why treating just one piece - like popping a pill for high blood sugar - rarely fixes the whole picture. You have to break the cycle at its source: belly fat.
Studies show that losing just 5-10% of your body weight reduces triglycerides by up to 40%, lowers blood sugar by 20-30%, and shrinks waist size by 5-8 inches. That’s not magic. That’s biology.

What Actually Works to Reverse It
There’s no pill that replaces movement, food, and sleep. But there are proven strategies:
- Move daily. Aim for 150 minutes of brisk walking, cycling, or swimming. Even 10-minute walks after meals help lower blood sugar spikes.
- Change your plate. Eat more vegetables, legumes, nuts, fish, and whole grains. Cut out sugary drinks, white bread, pastries, and processed snacks. The Mediterranean diet has been shown to cut heart events by 30% in people with metabolic syndrome.
- Limit alcohol. One drink a day for women, two for men. Alcohol spikes triglycerides and adds empty calories.
- Sleep 7-8 hours. Poor sleep raises cortisol, which increases belly fat and insulin resistance.
- Track your waist. Measure it every month. It’s a better indicator of progress than the scale.
Medications like metformin, statins, or fibrates may help in some cases - but they’re not a substitute. The NHLBI says: “Weight loss remains the most effective strategy for reversing all components of metabolic syndrome.”
What’s New in 2026
Doctors are starting to use something called the TyG index - a simple calculation: Ln(fasting triglycerides × fasting glucose ÷ 2). It’s a quick way to estimate insulin resistance without special tests. A score above 8.5 signals trouble.
Researchers are also looking at gut bacteria. People with metabolic syndrome have different microbiomes than healthy people. Future treatments might include targeted probiotics or fiber supplements to rebalance gut health.
The big shift? We’re moving from just diagnosing metabolic syndrome to measuring metabolic health - tracking blood sugar trends with continuous monitors, not just one fasting number. This gives a real-time picture of how your body responds to food, stress, and sleep.
What Happens If You Ignore It
If you have metabolic syndrome and do nothing, your odds of developing type 2 diabetes are 5 times higher. Your risk of heart disease doubles. And it doesn’t happen overnight. It creeps in over years - silent, slow, and sneaky.
But here’s the good news: if you act early, you can reverse it. Studies show that after 12 months of lifestyle changes, up to 50% of people no longer meet the criteria for metabolic syndrome. That’s not a miracle. That’s science.
You don’t need to be perfect. You just need to start. One less soda. One extra walk. One more hour of sleep. Small steps break the cycle.
Can you have metabolic syndrome if you’re not overweight?
Yes. Some people have a normal BMI but carry excess fat around their abdomen - known as TOFI (thin outside, fat inside). This fat is just as dangerous as visible belly fat. Waist size is a better indicator than weight alone.
Is metabolic syndrome the same as prediabetes?
No. Prediabetes is one part of metabolic syndrome - specifically, elevated fasting blood sugar. But metabolic syndrome includes at least three of five risk factors, including waist size, triglycerides, blood pressure, and cholesterol. You can have prediabetes without metabolic syndrome, and vice versa.
Can medications cure metabolic syndrome?
Medications can help manage individual pieces - like lowering blood pressure or blood sugar - but they don’t reverse the root cause: insulin resistance from abdominal fat. Only lifestyle changes - diet, movement, sleep - can truly reverse the syndrome. Drugs are support, not solutions.
How long does it take to reverse metabolic syndrome?
Signs of improvement can show up in as little as 4-6 weeks with consistent changes - like lower triglycerides or better fasting glucose. But full reversal usually takes 6-12 months. The key is consistency, not speed. Losing 5-10% of your body weight is enough to make a major difference.
Does alcohol cause metabolic syndrome?
Alcohol doesn’t cause it alone, but it’s a major contributor. It spikes triglycerides, adds empty calories, and worsens insulin resistance. Even moderate drinking - more than one drink a day for women or two for men - makes it harder to reverse the condition. Cutting back is one of the fastest ways to improve your numbers.
If you’ve been told you have metabolic syndrome, don’t panic. This isn’t a life sentence. It’s a signal - and you have more power to change it than you think. Start with your waist. Watch your sugar. Cut the junk. Move every day. Your future self will thank you.
Gina Beard
January 24, 2026 AT 22:15It’s not about willpower. It’s about biology. Your body isn’t broken-it’s adapting. And if you’re still blaming yourself for belly fat, you’re missing the point.
It’s not laziness. It’s insulin resistance.
And that’s not a moral failure. It’s a metabolic reality.
Karen Conlin
January 26, 2026 AT 14:42Y’all need to hear this: metabolic syndrome isn’t a life sentence-it’s a wake-up call wrapped in a waistline. I’ve seen clients go from prediabetic to thriving in 8 months just by swapping soda for sparkling water, walking after dinner, and sleeping like their life depends on it (because it does).
One woman, 58, 36-inch waist, normal BMI-she thought she was ‘fine.’ Then her triglycerides hit 280. She cried in my office. Then she started meal prepping. Now she hikes with her grandkids. No meds. Just movement. Just meals. Just consistency.
And yes, ethnicity matters. South Asian women? Watch your waist at 31 inches. Middle Eastern men? Your cutoff’s lower than you think. Global health isn’t one-size-fits-all. Stop comparing your insides to someone else’s outside.
This isn’t a diet. It’s a reset. And you don’t need to be perfect. You just need to show up. One walk. One less slice of bread. One more hour of sleep. That’s how revolutions start.
Josh McEvoy
January 27, 2026 AT 00:20bro i had a 42 inch waist and thought i was just "big boned" 😭
then my doc said "your liver is crying" and i lost 25 lbs in 3 months just cutting out soda and late night chips
now my triglycerides are normal and i can actually see my ankles 🤯
also i started sleeping 8 hrs and my mood is 1000% better
it’s not magic it’s just not being an idiot
Heather McCubbin
January 27, 2026 AT 13:51Everyone talks about diet and exercise like it’s some easy fix but nobody admits the truth-you’re not fighting fat you’re fighting decades of processed food addiction and corporate lies
Big Pharma doesn’t want you to reverse this they want you on metformin forever
And don’t get me started on how they market "low fat" as healthy when it’s just sugar in disguise
Wake up people your body is not a vending machine
Shanta Blank
January 29, 2026 AT 11:35Let me be the ugly truth here: if you’re still drinking fruit juice thinking it’s "healthy" you’re part of the problem.
It’s sugar. In liquid form. With a prettier label.
And if you think a 30-minute spin class cancels out three energy drinks a day-you’re not just deluded, you’re dangerous to your own health.
Stop romanticizing "balance."
Balance is for people who don’t want to change.
Real change is brutal. It’s saying no. It’s choosing sleep over scrolling. It’s cooking instead of ordering.
And if you can’t do that? Then stop pretending you care.
You don’t want to fix it. You want to feel better about not fixing it.
Amelia Williams
January 30, 2026 AT 14:44I’m 41, had metabolic syndrome at 190 lbs with a 38-inch waist-and I reversed it without surgery or drugs.
Here’s what helped: I started measuring my waist every Sunday. Not the scale. The tape.
I swapped white rice for cauliflower rice. Not because it’s trendy-because my blood sugar stopped spiking after lunch.
I walked 10 minutes after every meal. Even on rainy days. Even when I was tired.
And I stopped obsessing over calories. Started obsessing over how I felt.
6 months in, my triglycerides dropped 40%. My fasting glucose? Back in the normal range.
It’s not about being thin. It’s about being alive.
If I can do it, you can too. Just start small. One step. One meal. One sleep hour.
You’ve got this.
Viola Li
January 31, 2026 AT 03:05Interesting how this post ignores the role of chronic stress and cortisol-induced visceral fat accumulation
Also, the TyG index is not validated across all ethnic groups yet
And calling it a "vicious cycle" implies inevitability when socioeconomic factors like food deserts and shift work are the real drivers
Blaming individuals for metabolic syndrome is lazy science
Luke Davidson
February 1, 2026 AT 14:57Man I read this whole thing and I just wanna hug everyone who’s trying
It’s not easy. I know. I’ve been there.
Some days you eat clean and still feel like crap. Some nights you’re too tired to move.
But hear me: every time you choose water over soda, every time you take that walk even when you don’t feel like it-you’re not just changing your body.
You’re rebuilding your relationship with yourself.
And that’s the real win.
Don’t listen to the noise. Don’t compare your start to someone else’s middle.
Just keep showing up.
That’s enough.
You’re doing better than you think.
Sushrita Chakraborty
February 2, 2026 AT 20:49As someone from India, I appreciate the mention of ethnic thresholds. In South Asia, metabolic syndrome often manifests at BMI <23 and waist circumference as low as 31 inches for women-yet many clinicians still rely on Western criteria. This delay in diagnosis leads to premature cardiovascular events.
Additionally, traditional diets rich in millets, lentils, and ghee (in moderation) have shown protective effects in studies from Chennai and Mumbai. The problem isn’t just sugar-it’s the displacement of whole foods by refined carbohydrates and industrial oils.
Sleep is also undervalued: in cultures with late-night family routines and early work hours, chronic sleep deprivation exacerbates insulin resistance. A 7-hour sleep target is ideal, but even 6.5 hours with consistent timing helps.
Thank you for highlighting that reversal is possible. Hope this reaches more global communities.