More than 1 in 10 adults over 80 in the U.S. are taking prescription sleep meds every month. That’s not just a statistic-it’s someone’s parent, neighbor, or friend trying to get through the night. These drugs work-fast. But what happens when they stop working? Or when you can’t sleep without them? Or when you wake up groggy, confused, or even sleepwalking? The truth is, most people don’t know the real risks behind those little pills they’ve been popping for months-or years.
How Sleep Medications Actually Work
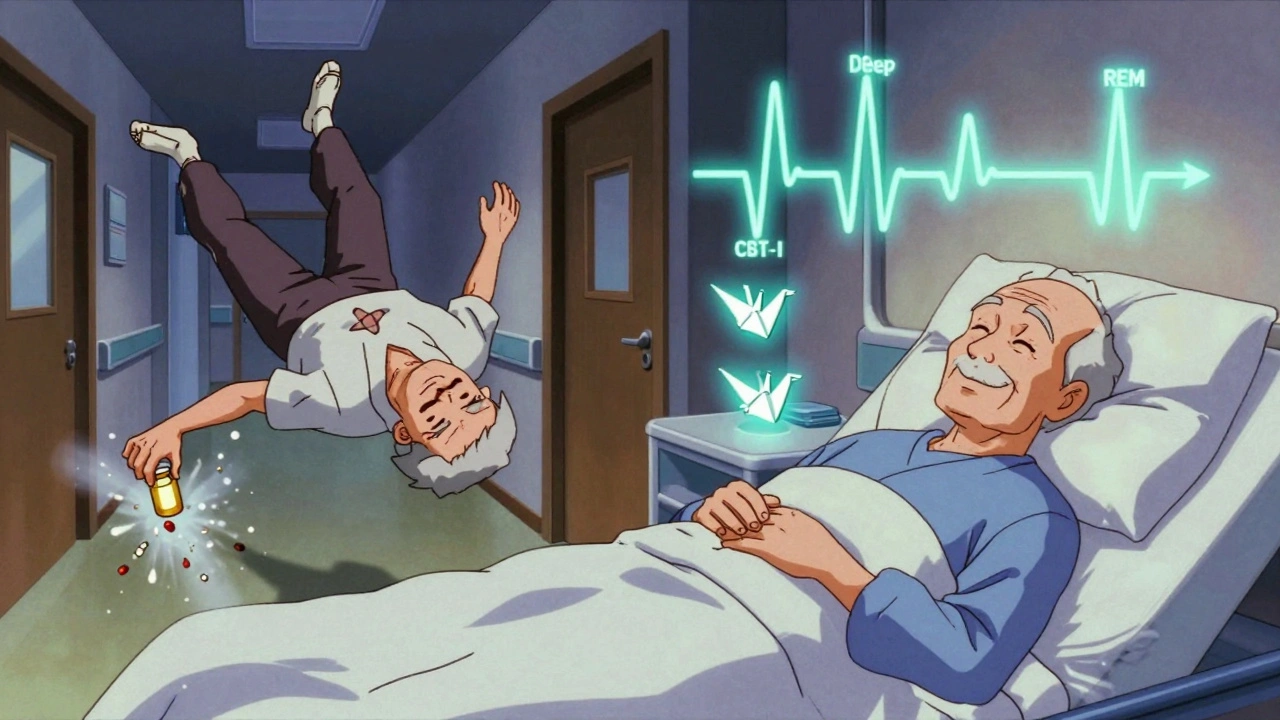
Sleep meds don’t make you tired. They slow down your brain. Most of them boost GABA, a calming neurotransmitter that tells your nervous system to chill out. That’s why you feel drowsy. But this isn’t natural sleep. Natural sleep cycles through light, deep, and REM stages. Medications like zolpidem (Ambien) or eszopiclone (Lunesta) force you into sleep, but they often flatten those cycles. You might sleep longer, but you’re not sleeping well.There are three main types:
- Benzodiazepines (like lorazepam or diazepam): These were the first sleep pills. They’re strong, but they carry a high risk of dependence-up to one-third of people who use them regularly for more than a month become dependent.
- Z-drugs (zolpidem, eszopiclone, zaleplon): Developed to be safer, these target specific GABA receptors. They’re faster acting and shorter-lived, but they still cause next-day drowsiness, memory lapses, and even sleep-driving. The FDA added a boxed warning to Ambien in 2019 after hundreds of reports of people waking up mid-drive.
- Off-label antidepressants (trazodone, doxepin): Often prescribed because they’re cheap. Trazodone can cause priapism (a painful, prolonged erection). Doxepin can mess with heart rhythms at higher doses.
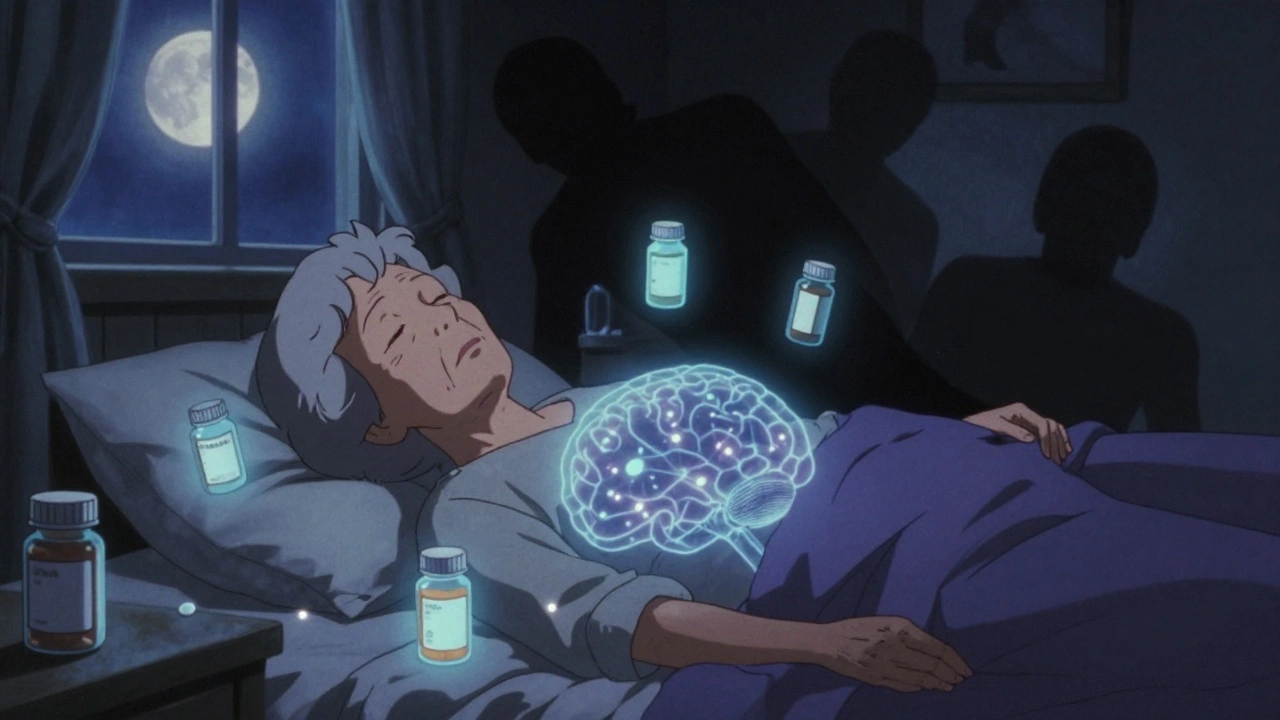
Even over-the-counter options like diphenhydramine (Benadryl) aren’t harmless. They block acetylcholine, a key brain chemical. Long-term use is linked to a 54% higher risk of dementia, according to a 2015 JAMA study. That’s not a myth. That’s data.
The Hidden Dangers: Dependence and Withdrawal
You think you’re just taking a pill to sleep. But your brain adapts. Over time, it needs more of the drug to get the same effect. That’s tolerance. Then comes withdrawal. Stop cold turkey? You might not sleep for days. Your body goes into overdrive-heart racing, anxiety soaring, insomnia worse than before.Studies show 5-10% of Z-drug users become dependent. Benzodiazepines? Up to 33%. And it’s not just physical. There’s psychological dependence too. You start believing you can’t survive the night without it. One Reddit user wrote: “After six months of nightly Ambien, I tried to quit. Couldn’t sleep for three nights. Ended up back on it.” That’s not weakness. That’s how these drugs rewire your brain.
Doctors often prescribe these for only 2-5 weeks. But in practice? Many patients stay on them for years. Why? Because stopping feels impossible. The American Academy of Sleep Medicine says CBT-I should be the first step-not the last. But too many patients never even hear about it.

Who’s at Greatest Risk?
It’s not just older adults. Though they’re the biggest users-13.2% of those 80+ take sleep meds-it’s the elderly who are most vulnerable. The American Geriatrics Society’s Beers Criteria (2023) says these drugs should be avoided in people over 65. Why? Three big reasons:- Falls: Sleep meds increase fall risk by 50-60%. A single night of dizziness can mean a broken hip.
- Fractures: Older adults on these drugs have a 20-30% higher chance of breaking a bone.
- Cognitive decline: Even short-term use can blur thinking, slow reaction time, and mimic a blood alcohol level of 0.05-0.08%. That’s legally impaired in most places.
Women are 50% more likely to be prescribed these meds than men. Why? Partly because they report insomnia more often. But also because they metabolize zolpidem slower. That’s why the FDA lowered the starting dose for women from 10mg to 5mg in 2019. Yet many prescriptions still start too high.
The Real Alternative: CBT-I
There’s a treatment that works better than any pill-and has zero side effects. It’s called Cognitive Behavioral Therapy for Insomnia, or CBT-I. It’s not a magic trick. It’s a structured program that teaches you how to fix your sleep habits, thoughts, and environment.Here’s what it does:
- Stops you from lying in bed awake for hours
- Rebuilds your body’s natural sleep drive
- Reduces anxiety about not sleeping
- Teaches you how to wind down properly
Studies show CBT-I helps 70-80% of people. And the results last. Unlike pills, you don’t relapse when you stop. WebMD found 78% of users who tried CBT-I had better long-term sleep than those who relied on meds. But here’s the catch: 65% say it’s hard to start. It takes 4-8 weeks. You have to track your sleep. You have to stop napping. You have to get up at the same time every day-even if you didn’t sleep.
That’s why so many people give up. But digital versions now exist. The FDA approved Somryst in 2020-a prescription app that delivers CBT-I through your phone. In trials, 60% of users achieved full remission of insomnia. No pills. No dependence.
New Options on the Horizon
There’s a new class of drugs called orexin receptor antagonists. Daridorexant (brand name Quviviq), approved in January 2022, works differently. Instead of sedating your brain, it blocks the chemical that keeps you awake. The result? Better sleep without the next-day fog. In clinical trials, users reported only 2.1 on a residual impairment scale-compared to 3.8 for zolpidem.And melatonin? It’s not a drug. It’s a hormone your body makes naturally. Taking it as a supplement helps reset your clock, especially if you’re jet-lagged or have delayed sleep phase. It’s not a cure for chronic insomnia, but it’s safer than anything that sedates you. Amazon reviews show 4.2/5 stars-mostly because users say they wake up feeling clear-headed.
What You Should Do Right Now
If you’re on sleep meds and want to stop:- Don’t quit cold turkey. That’s dangerous. Talk to your doctor about a taper plan-usually 25% reduction every two weeks.
- Ask for a referral to CBT-I. Many insurance plans cover it now. If your doctor doesn’t know where to send you, search for accredited providers through the American Academy of Sleep Medicine.
- Try a digital CBT-I app like Somryst. It’s FDA-cleared and available by prescription.
- If you’re over 65, ask your doctor to review every medication on your list. Sleep meds should be on the top of the “stop” list.
- Track your sleep for a week before your appointment. Note what time you get in bed, how long it takes to fall asleep, how many times you wake up, and how you feel in the morning.
If you’re thinking about starting sleep meds:
- Ask: “Is this my only option?”
- Ask: “What happens if I take this for 6 months?”
- Ask: “Can I try CBT-I first?”
There’s no shame in needing help. But there’s real risk in choosing the quickest fix. Sleep is too important to gamble with.
Can sleep medications cause memory loss?
Yes. Z-drugs like Ambien and Lunesta are linked to short-term memory gaps and even sleepwalking or sleep-driving episodes. These aren’t rare-FDA reports show about 0.5% of users experience complex sleep behaviors. Long-term use of anticholinergic OTC meds like Benadryl is tied to a 54% higher risk of dementia, according to JAMA Internal Medicine. Even occasional use can cause confusion, especially in older adults.
How long can you safely take sleep pills?
Clinical guidelines say 2-5 weeks max. Beyond that, effectiveness drops, and risks rise. Tolerance builds quickly. Dependence can start in as little as 3-4 weeks with benzodiazepines. Even Z-drugs lose their edge after four weeks. The goal isn’t to sleep forever on pills-it’s to use them as a bridge to better sleep habits.
Is melatonin safer than prescription sleep aids?
Generally, yes. Melatonin is a hormone your body naturally produces to signal bedtime. It doesn’t sedate you-it helps align your internal clock. It’s not a cure for chronic insomnia, but it’s much safer than drugs that depress your central nervous system. No dependence. No next-day grogginess. No fall risk. Just don’t take high doses (1-3 mg is enough). More isn’t better.
Why do doctors still prescribe sleep meds if they’re risky?
Because they’re fast, easy, and patients ask for them. Many doctors haven’t been trained in CBT-I. Insurance often doesn’t cover it well. And for someone in acute distress-say, after a loss or during a major life change-sleep meds can be a temporary lifeline. But they’re not meant to be long-term. The problem is, many patients never get referred to behavioral therapy, and the prescription becomes routine.
What should I do if I think I’m dependent on sleep medication?
Don’t stop suddenly. Talk to your doctor or a sleep specialist. Ask for a taper plan-usually reducing your dose by 25% every two weeks. Consider joining a CBT-I program. Many people find that once they learn how to sleep naturally, they don’t miss the pills. Support groups, like those on Reddit’s r/insomnia, can also help you feel less alone. You’re not weak for needing help. You’re smart for seeking a better way.
vinoth kumar
December 2, 2025 AT 05:44Finally, someone laid this out without sugarcoating. I’ve seen my uncle go from 5mg Ambien to 20mg just to get 4 hours of that zombie sleep. He didn’t even realize he was sleep-driving until he totaled his truck. No one warned him. Just a script and a shrug.
shalini vaishnav
December 3, 2025 AT 20:01This article is laughably naive. You act like CBT-I is some revolutionary cure-all while ignoring the structural collapse of mental healthcare in the West. In India, we don’t have access to digital apps or licensed therapists. We have pharmacies selling benzodiazepines over the counter. Your privileged Western solutions mean nothing to the global majority.
bobby chandra
December 5, 2025 AT 14:39Let me tell you something-sleep is the ultimate biohack. You’re not just losing sleep, you’re losing cognitive bandwidth, emotional resilience, and metabolic efficiency. These pills? They’re not just dangerous-they’re an insult to human biology. CBT-I isn’t therapy, it’s retraining your nervous system to remember how to rest. And yeah, it’s hard. But so is walking after a stroke. That doesn’t mean you don’t try.
I’ve coached 17 clients through CBT-I. Zero relapses. Zero dependence. One woman went from 12 hours in bed to 6 hours of real, restorative sleep. She cried the first morning she woke up without a pill. Not from sadness-from awe.
Archie singh
December 7, 2025 AT 08:30Of course the FDA warns about sleep-driving-because the pharmaceutical industry knew this all along and still pushed these drugs. You think this is about health? No. It’s about profit. Z-drugs are billion-dollar cash cows. CBT-I? No patent. No quarterly earnings. That’s why your doctor never mentioned it. He’s paid to prescribe, not to educate. Wake up. They’re selling you a chemical leash and calling it freedom.
Gene Linetsky
December 7, 2025 AT 17:15Did you know the FDA’s sleep-driving reports are underreported by 80%? They don’t count it if you don’t crash. And why? Because the drug companies own the data. I’ve got a cousin who sleep-drove to a 7-Eleven, bought a Slurpee, and drove back home without remembering any of it. He woke up with ice cream on his shirt. The doctor just wrote it off as 'sleep inertia.' Bullshit. This is a cover-up. They’re drugging the elderly so they don’t ask questions about their meds. And now they want you to trust their 'digital CBT-I app'? Please. That’s just another pill in app form.
Ignacio Pacheco
December 8, 2025 AT 11:35So melatonin’s safe because it’s ‘natural’? Interesting. So is arsenic. Natural doesn’t mean harmless. And the 1-3mg recommendation? That’s not based on science-it’s based on what’s cheap to manufacture. I’ve seen people take 10mg just to feel ‘something’-and then they’re groggy for 12 hours. This whole ‘natural alternative’ narrative is just marketing dressed up as wisdom.
Jim Schultz
December 9, 2025 AT 03:27Let’s be real: this entire system is a scam. Doctors are overworked, underpaid, and pressured to ‘solve’ insomnia with a script because they have 8 minutes per patient. Meanwhile, CBT-I requires 6-8 sessions, billing codes are terrible, and insurance refuses to cover it unless you’ve already failed 3 meds. So yeah, people stay on Ambien for 12 years. Not because they’re weak-because the system is rigged. And now you want to blame the patient? Please. The real villain is the healthcare industrial complex.
Kidar Saleh
December 10, 2025 AT 08:34I’m from London, and I’ve seen this play out in the NHS. A 78-year-old woman came in with chronic insomnia after her husband passed. She was on 10mg of zopiclone for three years. We didn’t just taper her-we walked her through sleep hygiene, journaling, light exposure, and breathwork. Took six months. She cried when she slept through the night without a pill. Said it felt like ‘remembering how to be human again.’ That’s the real win. Not the pill. Not the app. The reclamation of self.
Chloe Madison
December 10, 2025 AT 21:09