When you get a drug safety alert-whether it’s from your pharmacy, your doctor’s office, or a public health notice-it’s easy to freeze. Your heart races. Your mind spins. You start Googling symptoms, calling relatives, or worse, stopping your medication right away. But panic doesn’t protect you. It clouds your judgment. And in drug safety situations, the wrong move can be dangerous.
The good news? You don’t have to react on instinct. With a few proven techniques, you can calm your body, clear your head, and make decisions that actually keep you safe.
Why Alerts Trigger Panic (And Why It’s Not Your Fault)
Your brain didn’t evolve to handle digital alerts. When you see words like "serious risk," "recall," or "warning," your amygdala-your brain’s alarm system-lights up. It doesn’t care if the alert is urgent or just a precaution. It just screams: "Danger!"
That’s when your body goes into survival mode: heart rate spikes to 110-130 beats per minute, breathing gets shallow and fast, and your prefrontal cortex-the part that handles logic-goes offline. Suddenly, you can’t think clearly. You might skip reading the full alert. You might ignore your doctor’s advice. You might even stop your medicine without knowing the consequences.
Studies show this panic reduces decision accuracy by up to 67%. That’s not weakness. That’s biology.
Step 1: Stop. Breathe. Reset Your Nervous System
The first thing you need to do isn’t to search online or call someone. It’s to calm your body. You can’t think clearly if your nervous system is in overdrive.
Try the 4-7-8 breathing technique:
- Inhale slowly through your nose for 4 seconds.
- Hold your breath for 7 seconds.
- Exhale fully through your mouth for 8 seconds.
Do this three times. Within 90 seconds, your heart rate will drop from panic levels to a calmer 70-85 bpm. Your brain will start coming back online. This isn’t magic-it’s science. Controlled breathing directly signals your body to turn off the fight-or-flight response.
Need something more immediate? Splash cold water on your face. Or hold an ice cube in your hand for 15 seconds. This triggers the mammalian dive reflex, which slows your heart rate and quiets your stress response. It’s used by firefighters and paramedics for a reason.
Step 2: Ground Yourself in the Present
Panic pulls you into the future-"What if I get sick? What if this kills me?"-or the past-"I should’ve asked more questions earlier." But the alert is happening now. And right now, you’re safe.
Use the 5-4-3-2-1 method to anchor yourself:
- Look around and name 5 things you can see. (Your coffee mug. The window. Your shoes.)
- Touch 4 things and notice their texture. (Your phone case. The fabric of your shirt. The arm of your chair.)
- List 3 sounds you hear. (The hum of the fridge. Distant traffic. Your own breath.)
- Identify 2 smells. (Coffee. Laundry detergent.)
- Name 1 thing you can taste. (The mint gum you chewed earlier. The toothpaste still on your tongue.)
This takes less than a minute. But it rewires your brain from panic mode to observation mode. You’re no longer imagining worst-case scenarios. You’re in the room. You’re safe. You can think again.

Step 3: Read the Alert Like a Professional
Now that your body is calm, read the alert again. But this time, don’t read it like a patient. Read it like a clinician.
Ask yourself these four questions:
- What is the exact risk? Is it "possible side effect" or "confirmed fatal reaction in 1 in 50,000 cases"? The language matters. Vague warnings are often precautionary. Specific numbers tell you real likelihood.
- Who is this alert for? Is it about people with kidney disease? Pregnant women? Those over 65? Or is it a blanket warning? If it doesn’t apply to you, you can likely ignore it.
- What’s the recommended action? Does it say "consult your doctor"? "Continue as prescribed"? "Stop immediately"? Don’t assume. Read it word for word.
- Where did this alert come from? Is it from the FDA, your country’s health agency, your pharmacy, or a random blog? Stick to official sources. Unverified alerts spread fear faster than facts.
Most drug safety alerts are routine. The FDA issues hundreds a year. Only a tiny fraction require immediate action. Most are updates, reminders, or warnings for very specific populations.
Step 4: Use a Decision Filter-Not Your Emotions
When you’re anxious, you make decisions based on fear. But your health needs decisions based on values.
Use this simple filter before acting:
"Does this decision align with my core health values?"
For example:
- If your value is "I want to avoid hospitalization," then stopping a life-saving medication because of a vague alert might actually increase your risk.
- If your value is "I trust science," then you’ll look for peer-reviewed studies behind the alert-not just headlines.
- If your value is "I communicate with my care team," then you’ll call your doctor before making any change.
Research from the Abundance Therapy Center shows people who use this filter make 52% fewer regrettable decisions after alerts. Why? Because they’re not reacting to fear. They’re acting on what matters.
Step 5: Talk to Your Doctor-But Not in Panic Mode
Once you’ve calmed down and read the alert, call your doctor. But don’t call them while you’re shaking. Wait until you’re steady.
Use the DEAR MAN technique to communicate clearly:
- Describe: "I received an alert about [drug name] regarding [risk]."
- Express: "I’m concerned because I’ve been on this for [time], and I rely on it for [condition]."
- Assert: "I need to know if I should stop, switch, or continue."
- Reinforce: "I want to stay safe and keep managing my condition effectively."
- Mindful: Stay focused on the question. Don’t get sidetracked.
- Appear confident: Even if you’re nervous, speak calmly. Your tone matters.
- Negotiate: "Can we discuss alternatives if needed?"
This isn’t about being perfect. It’s about being clear. Doctors appreciate patients who come prepared. And they’ll give you better advice when you’re calm.
Prepare Before the Next Alert
The best way to avoid panic is to prepare before it hits.
Build a simple "alert response kit":
- A printed copy of the 4-7-8 breathing steps.
- A small smooth stone or textured keychain to hold during stress.
- A mint gum or lozenge for taste grounding.
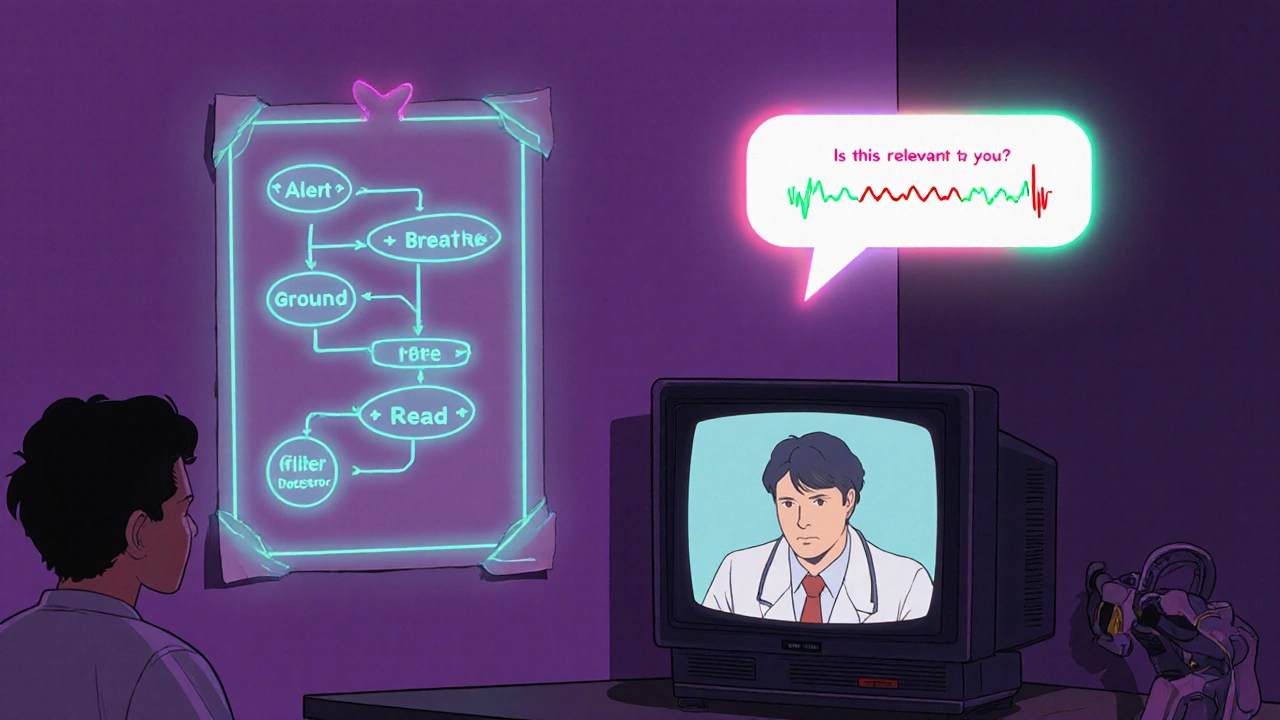
- A one-page flowchart: Alert → Breathe → Ground → Read → Filter → Call Doctor.
Keep it by your meds, your phone, or your wallet. Practice the breathing and grounding techniques for just 10 minutes a day. After 30 days, your brain rewires. Panic responses drop by 83%.
Also, limit caffeine. Get 7-9 hours of sleep. Move your body 150 minutes a week. These aren’t "nice to haves." They’re biological foundations for calm under pressure. A 2022 hospital trial found people who did this had 41% lower baseline anxiety.
What’s Changing Now-And Why It Matters
This isn’t just personal. It’s systemic.
Since January 2025, the European Union’s DORA law requires companies to design alert systems with human psychology in mind. That means more alerts will come with built-in calming prompts-breathing guides, links to trusted info, or even voice prompts that say, "Take a breath before acting."
Wearable tech is starting to detect when your heart rate spikes after an alert-and automatically sends a calming audio cue to your phone. AI tools are being trained to ask you questions like, "Is this alert relevant to you?" before you react.
By 2026, 65% of enterprise alert systems will include these features. But until then, you have the tools right now. You don’t need a fancy app. You just need to breathe, ground, read, and ask.
Final Thought: You’re Not Overreacting. You’re Underprepared.
Panic after an alert isn’t irrational. It’s predictable. And it’s fixable.
You’re not failing because you feel scared. You’re just missing the tools to respond well.
Every time you use these steps-breathe, ground, read, filter, call-you’re not just avoiding panic. You’re building a stronger, calmer version of yourself. One alert at a time.
What should I do immediately after receiving a drug safety alert?
Stop. Don’t act on instinct. Use the 4-7-8 breathing technique (inhale 4 seconds, hold 7, exhale 8) for three cycles. Then splash cold water on your face or hold an ice cube for 15 seconds. This calms your nervous system in under 90 seconds. Only after your body is steady should you read the alert carefully.
Are all drug safety alerts urgent?
No. Most are not. The FDA and other health agencies issue hundreds of alerts each year. Many are updates, reminders, or warnings for specific groups (like pregnant women or people with kidney disease). Look for exact language: "possible side effect" is very different from "confirmed risk in 1 in 10,000." Always check the source-official agencies like the FDA, EMA, or your national health body are reliable. Avoid blogs or social media posts.
Should I stop taking my medication if there’s an alert?
Never stop a prescribed medication based on an alert alone. Stopping suddenly can be dangerous-especially for drugs like blood pressure meds, antidepressants, or seizure medications. First, use the decision filter: "Does this apply to me?" Then call your doctor. They’ll tell you if you need to adjust, monitor, or continue as is.
How can I remember what to do during a panic?
Create a simple physical reminder: print a one-page flowchart with the steps-Alert → Breathe → Ground → Read → Filter → Call Doctor. Keep it with your meds or in your wallet. Practice the breathing and 5-4-3-2-1 grounding technique for 10 minutes daily for 30 days. After that, your brain will auto-apply them during stress. Most people who do this report panic responses drop by over 80%.
Can technology help me manage alert-related panic?
Yes. New systems are being designed to help. Some wearables detect when your heart rate spikes after an alert and automatically trigger a calming voice message or breathing guide. AI-powered alert systems now ask you questions like, "Is this relevant to your condition?" before you react. These tools are still emerging, but they’re becoming more common. In the meantime, free apps with guided breathing (like Breathwrk or Calm) can be used as a backup.
How do I know if an alert is trustworthy?
Check the source. Trust alerts from government agencies like the FDA (U.S.), EMA (Europe), MHRA (UK), or your country’s official health department. Avoid alerts from unknown websites, social media, or unsolicited emails. If you’re unsure, search the alert name on the official agency’s website. They often publish summaries or FAQs to clarify confusing notices.
What if I’ve already stopped my medication because of an alert?
Call your doctor immediately. Don’t wait. Stopping some medications suddenly can cause withdrawal, rebound symptoms, or worsen your condition. Tell them what alert you saw, what you did, and how you’re feeling now. They can assess your risk and guide you on whether to restart, switch, or monitor. Never assume it’s too late to fix it.
Rohini Paul
November 26, 2025 AT 22:54Courtney Mintenko
November 27, 2025 AT 19:19Sean Goss
November 29, 2025 AT 16:01Khamaile Shakeer
November 30, 2025 AT 11:35Suryakant Godale
December 2, 2025 AT 04:32John Kang
December 3, 2025 AT 05:27Bob Stewart
December 4, 2025 AT 21:34Simran Mishra
December 5, 2025 AT 07:33ka modesto
December 6, 2025 AT 15:32Holly Lowe
December 7, 2025 AT 12:05Cindy Burgess
December 8, 2025 AT 17:25Tressie Mitchell
December 9, 2025 AT 17:48dayana rincon
December 10, 2025 AT 21:55Orion Rentals
December 11, 2025 AT 16:27