Beta-Blocker & CCB Combination Risk Calculator
Patient Risk Assessment
Combining beta-blockers and calcium channel blockers sounds like a smart move-two powerful heart medications working together to lower blood pressure, ease angina, or control arrhythmias. But this isn’t just about adding more power. It’s about cardiac effects that can turn helpful into dangerous in a matter of days if you don’t know what you’re doing.
How These Drugs Work (And Why They’re Combined)
Beta-blockers, like metoprolol and atenolol, slow your heart down. They block adrenaline’s effect on the heart, lowering heart rate, reducing blood pressure, and decreasing how hard the heart pumps. Calcium channel blockers, such as amlodipine and diltiazem, relax blood vessels by stopping calcium from entering muscle cells in the heart and arteries. This lowers blood pressure too-but some types also slow the heart’s electrical signals.
When used alone, both classes are effective. But when combined, their effects can add up. That’s why doctors sometimes use them together: for patients with high blood pressure that won’t budge with one drug, or for those with angina who also have a fast heart rate. The idea is simple-get better control with lower doses of each. But the reality? It’s a tightrope walk.
The Big Divide: Dihydropyridines vs. Non-Dihydropyridines
Not all calcium channel blockers are the same. This is the single most important thing to understand before mixing them with beta-blockers.
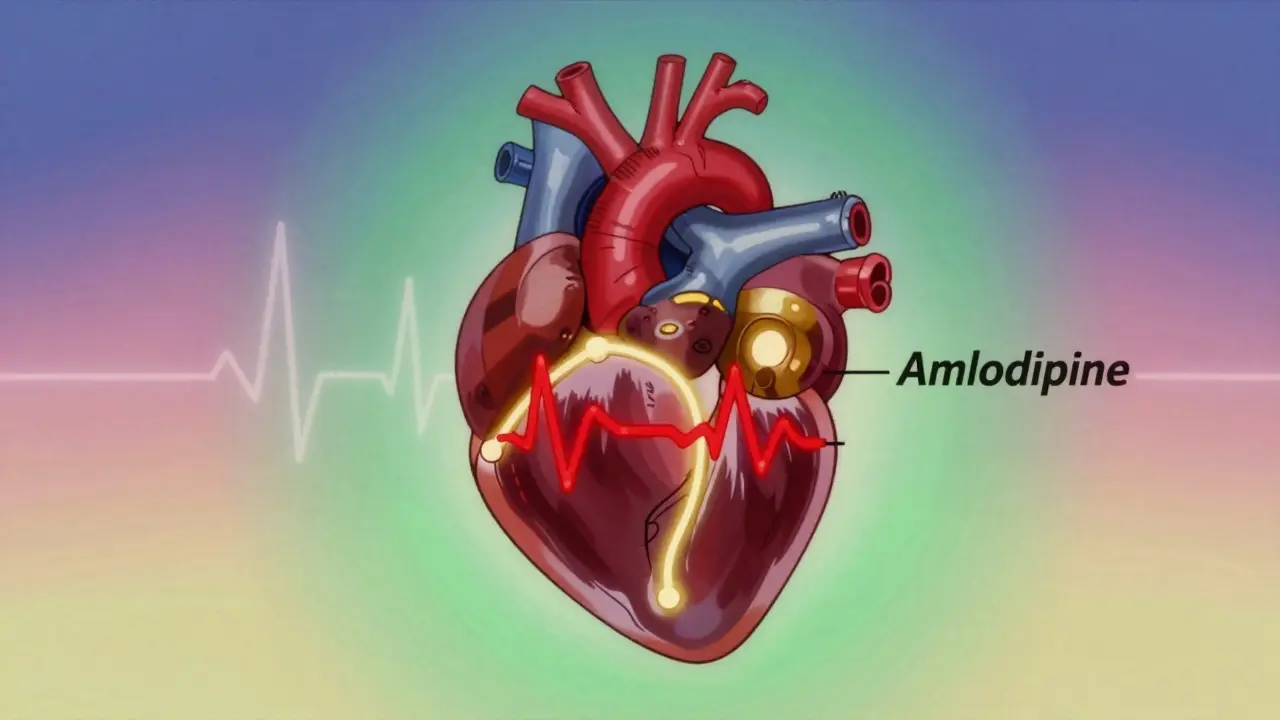
Dihydropyridines-like amlodipine, nifedipine, and felodipine-mainly target blood vessels. They cause vasodilation without much effect on the heart’s rhythm or pumping ability. When paired with a beta-blocker, this combo is generally safe and effective. In fact, studies show BB + amlodipine reduces stroke risk by 22% and heart failure risk by 28% compared to other dual therapies.
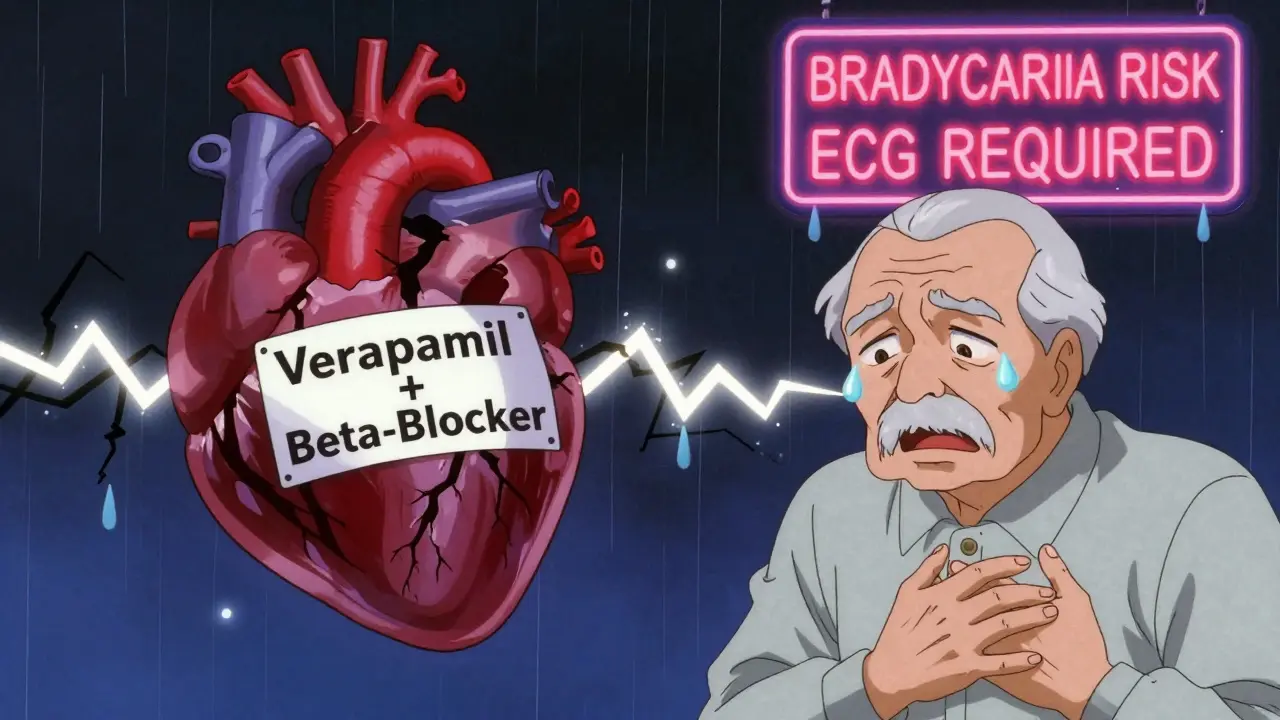
Non-dihydropyridines-verapamil and diltiazem-are different. They directly affect the heart’s electrical system. They slow conduction through the AV node, reduce contractility, and lower heart rate. Combine those with a beta-blocker, and you’re stacking two drugs that both suppress the heart’s natural pacemaker.
That’s where things get risky.
The Hidden Dangers: When Combination Therapy Turns Dangerous
In 2023, a study of nearly 19,000 Chinese hypertensive patients found that verapamil plus beta-blockers caused dangerous bradycardia or heart block in 10-15% of cases. That’s not rare. That’s common enough to warrant a red flag on every prescription.
Here’s what can happen:
- Heart rate drops below 50 bpm-sometimes below 40.
- PR interval on ECG stretches beyond 200 milliseconds, signaling delayed electrical signals.
- Left ventricular ejection fraction drops by 15-25% in patients with existing heart weakness.
- Complete heart block can occur, requiring emergency pacing.
A Reddit post from a cardiologist in 2023 described losing a patient to complete heart block after adding verapamil to metoprolol in an 82-year-old with a borderline PR interval. The comment had over 140 upvotes. Why? Because it’s not an outlier. It’s a warning many doctors are now taking seriously.
Even diltiazem, often seen as "milder" than verapamil, increases the risk of left ventricular dysfunction by 25% in patients with ejection fraction under 45%. That’s not a risk you take lightly.
Who Should Avoid This Combo?
The guidelines are clear. The 2018 ESC/ESH hypertension guidelines and the 2021 FDA boxed warning both say: avoid beta-blocker + verapamil/diltiazem combinations if you have:
- Sinus node dysfunction (sick sinus syndrome)
- Second- or third-degree AV block (unless you have a pacemaker)
- PR interval longer than 200 ms
- Heart failure with reduced ejection fraction (HFrEF)
- Age over 75 with no prior cardiac evaluation
And even if you don’t have those, you need screening. Before starting this combo, you need:
- A baseline ECG to check PR interval and heart rhythm
- An echocardiogram to measure ejection fraction
- Review of all other meds-especially other heart rate-lowering drugs
Many doctors skip these steps. That’s how bad outcomes happen.
When the Combo Actually Works-And Why
It’s not all bad news. When done right, BB + amlodipine is one of the most effective dual therapies for hypertension, especially in patients with angina.
Dr. Sarah Chen, a cardiologist at Massachusetts General Hospital, says she’s prescribed this combo to over 200 patients. Only 3% developed ankle swelling-manageable by lowering the amlodipine dose. No one had serious bradycardia. Why? Because she avoided non-dihydropyridines.
Studies back this up. The 2022 AHA analysis showed BB + amlodipine had a 3.2-fold lower risk of symptomatic bradycardia needing a pacemaker compared to BB + verapamil in patients over 65. The 2023 NIH study found BB + dihydropyridine CCB reduced major cardiac events by 17% compared to other dual therapies.
It works best in patients with:
- Hypertension plus stable angina
- Resting heart rate above 80 bpm (per ESC guidelines)
- No history of conduction problems
- Normal kidney and liver function
It’s not a first-line choice for everyone-but for the right person, it’s a game-changer.
What About Side Effects Everyone Ignores?
Most people talk about heart rate. But there’s another problem: swelling.
Dihydropyridine CCBs like amlodipine cause peripheral edema in up to 22% of patients on combination therapy. That’s 35% higher than with ACE inhibitor combos. It’s not dangerous, but it’s annoying-and it leads to 18% of patients stopping the meds.
Also, drug interactions aren’t always obvious. Verapamil blocks a liver transporter called P-glycoprotein. In 30% of people with a genetic variant called CYP2D6 poor metabolizer status, this can increase beta-blocker levels by 20-30%. That means even if you’re on a low dose, your body might be getting a much higher dose than intended.
And don’t forget: if you’re on other meds-like statins, antifungals, or antidepressants-your risk goes up. Polypharmacy is the silent killer here.

What Do Doctors Actually Do?
A 2022 survey of 1,247 U.S. clinicians showed:
- 78% prefer BB + dihydropyridine CCB (like amlodipine)
- Only 12% would ever use BB + verapamil, even in select cases
- 63% said fear of bradycardia was their biggest reason to avoid the combo
- 89% said it was effective for angina + hypertension
Real-world practice is shifting. Hospitals like Kaiser Permanente cut adverse events by 44% after implementing strict protocols: mandatory ECG before prescribing, automated alerts in electronic records for high-risk patients, and follow-up visits at 7 and 30 days.
The European Society of Cardiology now offers an online risk calculator that predicts bradycardia risk with 89% accuracy. It asks for age, baseline heart rate, PR interval, ejection fraction, and other meds. It’s free. It’s simple. And too few doctors use it.
What Should You Do If You’re on This Combo?
If you’re taking beta-blockers and calcium channel blockers together:
- Know which type of CCB you’re on. Is it amlodipine? That’s fine. Is it verapamil or diltiazem? Ask your doctor why.
- Check your pulse daily. If it drops below 50 and you feel dizzy, lightheaded, or fatigued, call your doctor.
- Get an ECG if you haven’t had one in the last 6 months.
- Don’t skip follow-ups. The first month is critical-heart rate can drop slowly, without symptoms.
- Bring a full list of all your meds to every appointment-including OTC and supplements.
If you’re a patient over 65, or have any history of fainting, slow heart rate, or heart failure, this combo may not be right for you. Push for alternatives. There are plenty.
The Future of This Therapy
The market is changing. BB + amlodipine prescriptions are projected to grow 5.7% annually through 2028. BB + verapamil? Those are declining fast.
The 2024 European Society of Hypertension roadmap includes a new risk-stratification tool expected to launch in early 2025. It will help doctors decide who can safely use this combo-and who shouldn’t even try.
For now, the message is simple: this combination isn’t bad. But it’s not for everyone. And it’s not something to start without careful planning, testing, and monitoring.
Can beta-blockers and calcium channel blockers be taken together safely?
Yes-but only under specific conditions. Combining beta-blockers with dihydropyridine calcium channel blockers like amlodipine is generally safe and effective for hypertension and angina. Avoid combining them with non-dihydropyridines like verapamil or diltiazem unless you’ve had a full cardiac workup and have no conduction issues. Always start with low doses and monitor heart rate and ECG closely.
What are the most dangerous side effects of combining beta-blockers and calcium channel blockers?
The most dangerous side effects include severe bradycardia (heart rate below 50 bpm), heart block (especially second- or third-degree AV block), and worsening heart failure. These risks are highest with verapamil or diltiazem combined with beta-blockers. Symptoms like dizziness, fainting, extreme fatigue, or shortness of breath require immediate medical attention.
Is amlodipine safer than verapamil when used with a beta-blocker?
Yes, amlodipine is significantly safer. As a dihydropyridine calcium channel blocker, it primarily relaxes blood vessels without suppressing the heart’s electrical system. Verapamil, a non-dihydropyridine, directly slows heart rate and conduction, which can dangerously amplify the effects of beta-blockers. Studies show verapamil combinations increase the risk of pacemaker implantation by over 3 times compared to amlodipine combinations.
Who should never take beta-blockers with calcium channel blockers?
People with sinus node dysfunction, second- or third-degree heart block, PR interval longer than 200 milliseconds, heart failure with reduced ejection fraction (HFrEF), or a history of fainting should avoid this combination entirely. Elderly patients over 75 should also be screened carefully before starting, as undiagnosed conduction problems are common in this group.
Do I need an ECG before starting this combination?
Yes. A baseline ECG is essential to check your PR interval and heart rhythm. An echocardiogram to measure ejection fraction is also recommended, especially if you have any history of heart disease. Skipping these tests increases the risk of serious complications. Most guidelines now require them before initiating combination therapy.
What should I do if I feel dizzy or my heart feels slow after starting this combo?
Check your pulse immediately. If it’s below 50 bpm and you feel lightheaded, weak, or short of breath, stop taking the medication and contact your doctor right away. Do not wait for your next appointment. Severe bradycardia or heart block can develop quickly and may require emergency treatment. Keep a record of your pulse and symptoms to share with your provider.
Natasha Sandra
December 26, 2025 AT 01:47Sumler Luu
December 27, 2025 AT 04:03Sandeep Jain
December 27, 2025 AT 06:21Fabio Raphael
December 29, 2025 AT 00:02Amy Lesleighter (Wales)
December 30, 2025 AT 23:16Rajni Jain
January 1, 2026 AT 05:58sakshi nagpal
January 2, 2026 AT 09:02roger dalomba
January 4, 2026 AT 07:12Nikki Brown
January 6, 2026 AT 05:23Peter sullen
January 6, 2026 AT 18:16Becky Baker
January 7, 2026 AT 09:21Erwin Asilom
January 9, 2026 AT 02:19Brittany Fuhs
January 10, 2026 AT 20:06