Most people don’t realize their eyes are under pressure-until it’s too late. Glaucoma doesn’t hurt. It doesn’t blur your vision right away. But slowly, steadily, it kills the nerve cells that send images from your eye to your brain. By the time you notice, you’ve already lost up to 40% of your vision. And once it’s gone, it’s gone for good.
What Glaucoma Really Is
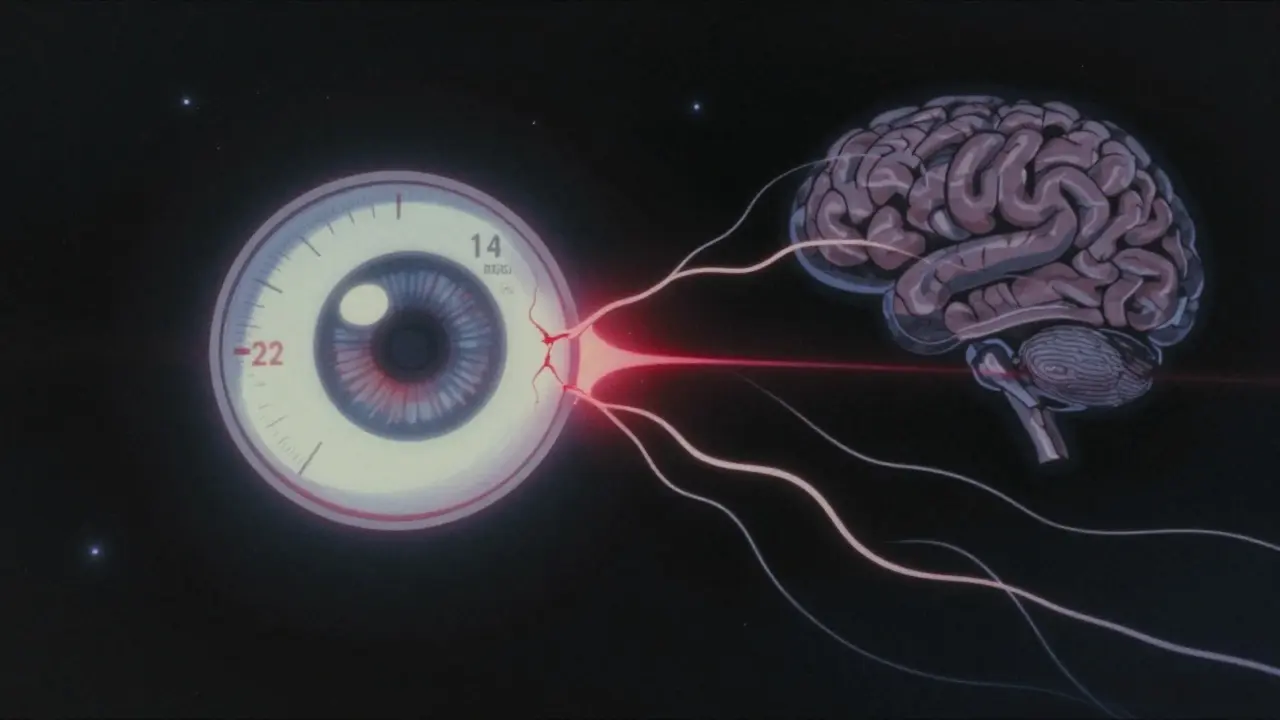
Glaucoma isn’t just high eye pressure. That’s the old story. The truth? It’s a slow, silent breakdown of the optic nerve, often triggered by pressure-but not always. The optic nerve is like a cable made of over a million tiny wires. Each wire carries a piece of what you see. When these wires start dying, your vision fades from the edges inward. You might miss a step. You might bump into things. You won’t know why.
Normal eye pressure, called intraocular pressure (IOP), sits between 10 and 21 mmHg. It’s measured with a quick puff of air or a gentle touch on the eye using the Goldmann tonometer-the gold standard. But here’s the catch: some people with pressures above 21 mmHg never develop glaucoma. Others with pressures below 15 mmHg lose vision anyway. That’s because pressure alone doesn’t tell the whole story.
The Real Culprit: Pressure Difference, Not Just Pressure
Think of your eye and your brain like two rooms connected by a thin wall. Your eye has pressure. Your brain has pressure too, from the fluid around it called cerebrospinal fluid. Glaucoma doesn’t just care about how hard the pressure is in your eye. It cares about the difference between the two.
Studies show that in normal-tension glaucoma, where eye pressure stays low, the pressure in the brain is often lower than it should be. That means the wall-the lamina cribrosa, a mesh-like structure at the back of the optic nerve-gets stretched. Over time, that stretch crushes the nerve fibers. In people with high eye pressure, the same thing happens, but faster. The pressure difference is what matters. That’s why someone with 22 mmHg in their eye and 14 mmHg in their brain is at higher risk than someone with 25 mmHg in their eye and 20 mmHg in their brain.
How Damage Happens: From Strain to Cell Death
When pressure pushes on the optic nerve head, it doesn’t just squeeze. It changes the structure. The lamina cribrosa, which normally acts like a shock absorber, gets pulled backward. In healthy eyes, this movement is tiny-about 3% strain. In glaucoma, it’s 30-50% more. That strain damages the tiny axons-the wires-that carry signals from the retina. These axons need constant support from nearby cells: astrocytes, microglia, and blood vessels. When the pressure imbalance lasts too long, those support cells fail. The axons stop working. Then they die.
And here’s the scary part: once a retinal ganglion cell dies, it doesn’t come back. No treatment can regrow it. That’s why catching glaucoma early is everything.
Types of Glaucoma You Need to Know
Not all glaucoma is the same. The most common type-making up 90% of cases in the U.S.-is primary open-angle glaucoma (POAG). It’s slow, sneaky, and painless. Eye pressure rises gradually, and damage happens over years.
Then there’s normal-tension glaucoma (NTG). It’s more common in Asian populations, where up to 70% of glaucoma cases happen without high pressure. People with NTG often have low blood pressure, sleep apnea, or Raynaud’s syndrome. Their optic nerves are just more sensitive.
Angle-closure glaucoma is rarer but dangerous. It happens when the iris blocks the drainage channel suddenly. Pressure spikes fast-sometimes to 40 or 50 mmHg. This can cause severe pain, nausea, and sudden vision loss. It’s an emergency.
Secondary glaucoma comes from other problems: steroid use, eye injuries, tumors, or inflammation. Pigmentary glaucoma happens when pigment from the iris flakes off and clogs drainage. Pseudoexfoliative glaucoma is caused by flaky material building up in the eye. Both can progress faster than open-angle glaucoma.
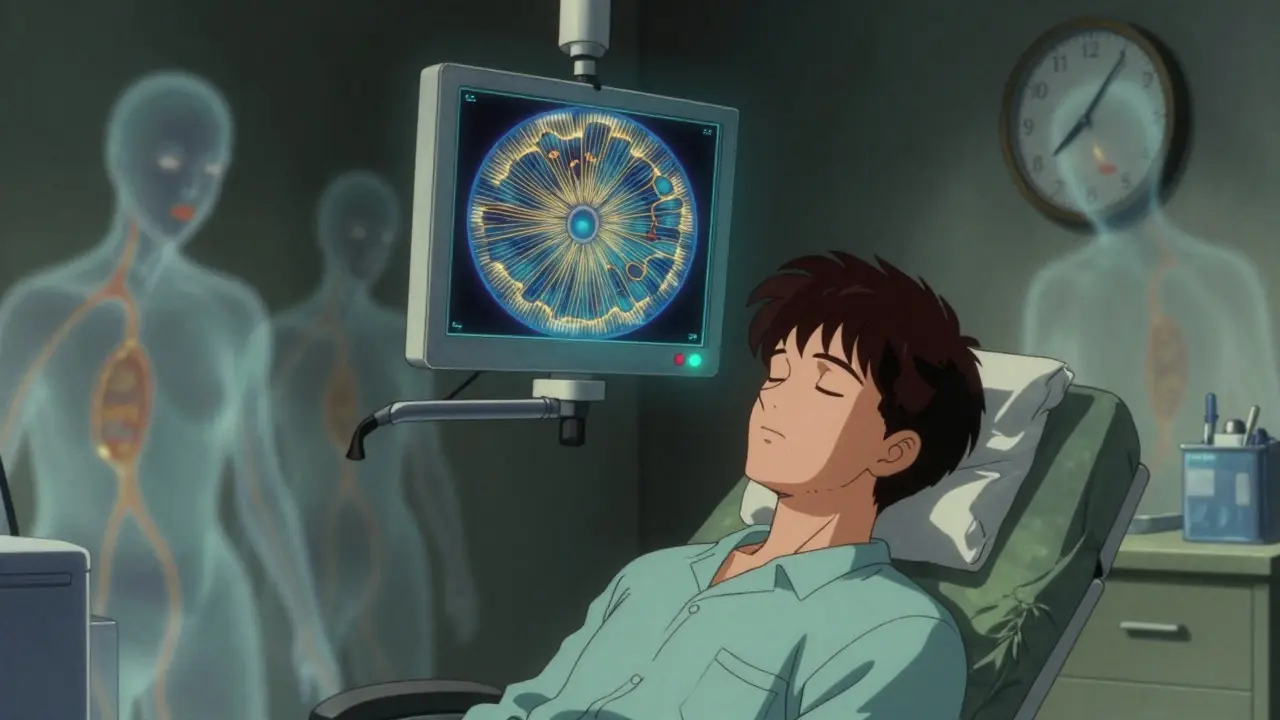
How Doctors Detect It Before It’s Too Late
There’s no symptom. No warning. That’s why screening matters. If you’re over 40, get checked. If you’re over 60, you should be checked every year.
Three tools do the heavy lifting:
- Optical Coherence Tomography (OCT) scans the retina in microns. It can spot thinning of the nerve fiber layer as small as 5 microns-years before you notice vision loss.
- Visual field testing (like Humphrey perimetry) maps where you can and can’t see. A 1 dB loss might seem tiny, but it’s the first sign of nerve damage.
- Fundus photography takes pictures of the optic disc. A larger cup-to-disc ratio means more damage.
These tests aren’t optional. They’re your lifeline. Skipping them is like ignoring a car’s check engine light.
Treatment: Lowering Pressure, Slowing Damage
There’s no cure. But there’s control. And control means preserving vision.
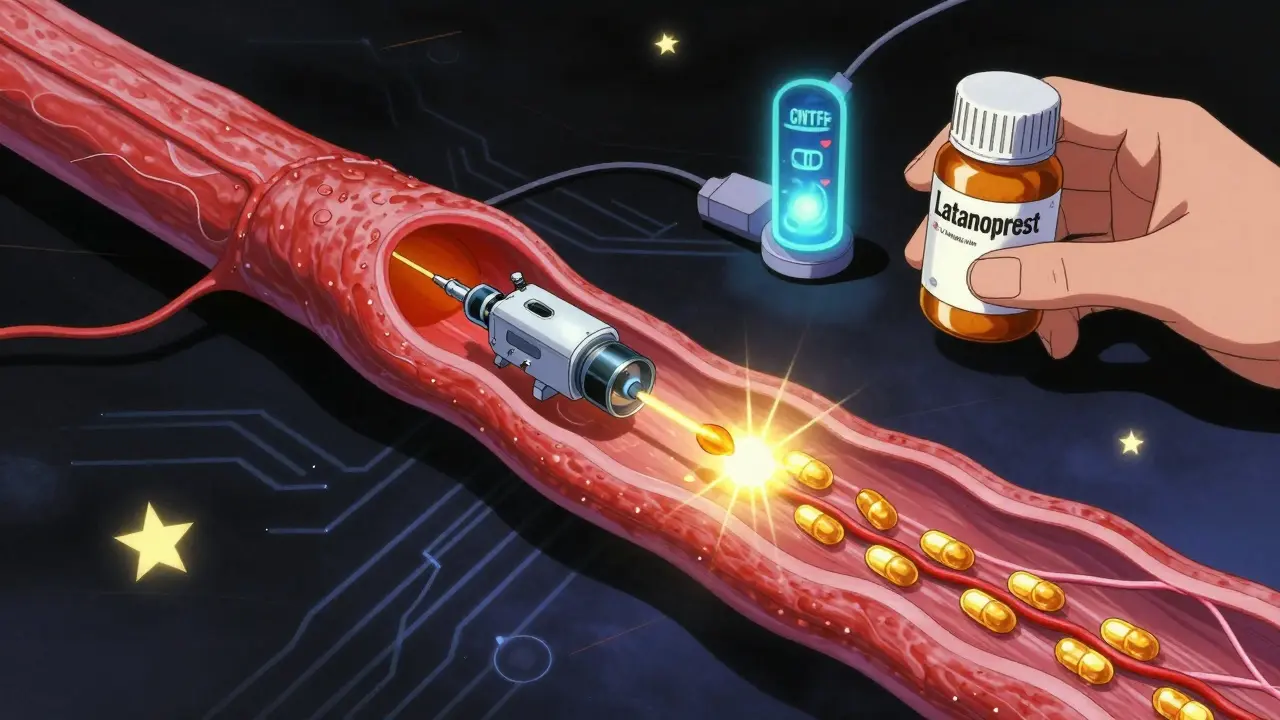
First-line treatment? Prostaglandin eye drops-like latanoprost. They work by opening the drainage channels. They lower pressure by 25-33% with just one drop a day. But side effects? Eyelashes grow longer. The skin around the eye can darken. Some people hate the redness.
If drops aren’t enough, laser treatment helps. Selective laser trabeculoplasty (SLT) targets the drainage system. It works in 75% of people, lowering pressure by 20-30%. But the effect fades over time. After five years, about half need another treatment.
Surgery is for advanced cases. Trabeculectomy creates a new drainage path. Success rates are high-85% in the first year. But complications like infection or scarring can happen. Newer minimally invasive glaucoma surgeries (MIGS), like iStent, are safer. They’re often done during cataract surgery. They lower pressure by 20-25% and reduce the need for drops.
Target pressure? It’s not one-size-fits-all. If you have severe damage, aim for 12-15 mmHg. Moderate? 15-18 mmHg. Mild? 18-21 mmHg. The goal is to cut pressure by 20-50% from your baseline. The Early Manifest Glaucoma Trial proved that reducing pressure by half cuts progression risk by 50%.
Why Adherence Is the Biggest Hurdle
Here’s the ugly truth: half of glaucoma patients stop their drops within a year. Why? Side effects. Forgetfulness. The false belief that “no symptoms = no problem.”
A 2022 survey of 1,200 patients found 42% had burning or redness that made them skip doses. Another 30% said they forgot. One Reddit user wrote: “I’ve had IOP at 13 for five years. My vision still gets worse. Why?” The answer? Pressure isn’t the only factor. Damage can creep on even when numbers look good.
That’s why support matters. Regular check-ins. Pill organizers. Apps that remind you. Talking to your doctor about side effects-not ignoring them.
What’s Next: Beyond Pressure
Scientists are no longer just lowering pressure. They’re trying to save the nerve itself.
In animal studies, a protein called oncomodulin helped regrow damaged optic nerve fibers by 40%. That’s not ready for humans yet-but it’s proof regeneration is possible.
The LIBERTI study found that brimonidine, a glaucoma drop, slowed progression in normal-tension glaucoma even when pressure didn’t drop much. That suggests it might protect nerves directly.
Other trials are testing CNTF implants-tiny devices that release growth factors into the eye. At two years, patients preserved 2.5 dB more vision than those on standard treatment.
Gene therapy is also in early trials. One method targets the eye’s drainage system to improve fluid flow. After six months, IOP dropped 25% without drops.
These aren’t magic bullets. But they’re signs we’re moving beyond just lowering numbers. We’re starting to heal.
What You Can Do Today
Glaucoma doesn’t care how healthy you are. It doesn’t care if you exercise, eat well, or meditate. It only cares about pressure, genetics, and time.
Here’s what actually works:
- Get your eyes checked every 1-2 years after 40. Every year after 60.
- If you have a family history, start at 35.
- Don’t ignore eye pressure checks-even if you feel fine.
- Take your drops like clockwork. Set alarms. Use a pill box.
- Ask your doctor about OCT and visual field tests. Don’t let them skip them.
- Know your numbers. Write them down. Track them.
There’s no guarantee you’ll never get glaucoma. But if you catch it early, you can keep your vision. And that’s worth more than any drop, laser, or surgery.
Can glaucoma be cured?
No, glaucoma cannot be cured. Once optic nerve cells are lost, they don’t regenerate. But with early detection and consistent treatment, progression can be slowed or stopped in most cases. The goal of treatment is to preserve remaining vision, not restore what’s already gone.
Is high eye pressure always a sign of glaucoma?
No. High eye pressure (above 21 mmHg) is a risk factor, but not a diagnosis. Some people have high pressure without any nerve damage-this is called ocular hypertension. Others have normal pressure but still develop glaucoma, known as normal-tension glaucoma. What matters is whether the optic nerve is damaged, not just the pressure number.
Can I feel glaucoma in my eyes?
In most cases, no. Glaucoma is silent. You won’t feel pain, pressure, or changes in vision until significant damage has occurred. The only exception is acute angle-closure glaucoma, which causes sudden pain, redness, nausea, and blurred vision. That’s a medical emergency.
Are eye drops the only treatment for glaucoma?
No. Eye drops are the first step, but not the only option. Laser treatments like SLT can reduce pressure by 20-30%. Surgery, such as trabeculectomy or MIGS procedures like iStent, is used when drops and lasers aren’t enough. The choice depends on severity, age, and how well you respond to treatment.
Why do I need so many eye tests?
Glaucoma changes slowly. A single test can’t show progression. OCT scans track thinning of the nerve layer. Visual field tests map blind spots. These changes are measured in microns and decibels-tiny shifts that add up over time. Regular testing lets your doctor know if your treatment is working or if it needs adjusting.
Can lifestyle changes prevent glaucoma?
Lifestyle changes alone won’t prevent glaucoma. But staying active, avoiding smoking, and managing blood pressure can help reduce risk. There’s no evidence that diet, supplements, or yoga prevent glaucoma. The only proven prevention is regular eye exams, especially if you’re over 40 or have a family history.