When your asthma symptoms don’t match your inhaler use, or your doctor can’t tell if your lungs are inflamed just by listening, there’s a simple test that gives real answers: FeNO testing. It’s not a lung function test like spirometry. It doesn’t require deep breaths or forceful blows. You just breathe slowly into a handheld device for 10 seconds-and in seconds, it tells your doctor how much inflammation is in your airways. This isn’t science fiction. It’s a proven tool used in clinics across the U.S. and Europe to make asthma care more precise.
What FeNO Testing Actually Measures
FeNO stands for Fractional Exhaled Nitric Oxide. Nitric oxide is a gas your body naturally produces, especially when there’s inflammation in your airways. In asthma, that inflammation is often driven by a type of immune response called type 2 inflammation, which involves eosinophils-white blood cells that swell up and irritate your breathing tubes. When these cells are active, they release more nitric oxide. The FeNO test catches that extra gas in your breath and measures it in parts per billion (ppb).
The test is easy. You inhale deeply through a filter that removes outside nitric oxide, then exhale steadily at a slow, constant rate-like blowing out a candle without puffing. The device reads your breath in real time and gives a number. For adults, a reading of 25 ppb or higher suggests significant airway inflammation. For kids aged 5 to 12, the cutoff is 20 ppb. These aren’t random numbers. They’re based on years of research and guidelines from the American Thoracic Society and GINA (Global Initiative for Asthma).
Why FeNO Matters More Than You Think
Many people with asthma are misdiagnosed-or worse, undertreated-because symptoms like wheezing and shortness of breath can look like other conditions: chronic bronchitis, acid reflux, even anxiety. Spirometry, the most common lung test, only shows if your airways are narrowed right now. It doesn’t tell you why they’re narrowed. That’s where FeNO steps in.
Studies show that high FeNO levels make an asthma diagnosis up to seven times more likely than spirometry alone. In one case documented by the American Lung Association, a 34-year-old patient had been treated for chronic bronchitis for seven years. Their FeNO level was 48 ppb. That confirmed asthma. They switched treatments-and their flare-ups dropped by 80%.
But FeNO isn’t just for diagnosis. It’s a tracking tool. If you’re on a steroid inhaler and your FeNO stays high, your medication isn’t working well enough. If your FeNO drops after starting a new biologic drug like dupilumab, it’s working. One patient on Reddit said: “Finally, objective proof my inhaler wasn’t working.” That’s the power of FeNO: turning guesswork into data.
How It Compares to Other Tests
Doctors have other ways to check for inflammation: blood tests for eosinophils, sputum analysis, even allergy skin tests. But each has limits.
- Blood eosinophil count (BEC): Shows inflammation in your blood, but not necessarily in your lungs. It correlates only moderately with airway inflammation.
- Sputum analysis: Requires coughing up mucus and sending it to a lab. It’s accurate but messy, time-consuming, and uncomfortable for many patients.
- Spirometry: Measures airflow, not inflammation. It can be normal even when inflammation is high, especially in early or mild asthma.
FeNO beats them all in simplicity and speed. It’s done in the office, takes under a minute, and works for kids as young as five. Unlike sputum tests, no special lab is needed. Unlike blood tests, it directly reflects what’s happening in your airways, not your bloodstream.
But FeNO isn’t perfect. It won’t catch non-eosinophilic asthma-where inflammation comes from other sources, like smoke or pollution. Smokers often have lower FeNO levels, even with active asthma. And if you’ve recently taken a steroid pill or shot, your FeNO might drop temporarily, giving a false sense of control.
When and How Often Should You Get Tested?
FeNO isn’t a one-time test. It’s a monitoring tool. Experts recommend testing every 3 to 4 months if you’re on maintenance therapy. If you’re adjusting your treatment-switching inhalers, starting a biologic, or dealing with worsening symptoms-your doctor might test you more often.
The test must be done right to be useful. You need to avoid eating, drinking (except water), smoking, or vigorous exercise for at least one hour before testing. You should also do FeNO before spirometry or using a rescue inhaler. If you blow too fast, too slow, or too short, the device will flag the result as invalid. Most modern devices, like the NIOX VERO®, give real-time feedback on your exhalation to help you get it right.
Invalid results happen in about 15-20% of first attempts. With practice and visual coaching from the machine, that drops to under 5%. Most patients, including children, find it easier than spirometry.
What the Numbers Mean
FeNO results are broken into three tiers:
- Low: under 25 ppb (adults) - Suggests little to no eosinophilic inflammation. Your asthma may be well-controlled or not driven by type 2 inflammation.
- Medium: 25-50 ppb - Moderate inflammation. You might benefit from a steroid inhaler or a step-up in treatment.
- High: over 50 ppb - Significant inflammation. This often means you’re at higher risk for flare-ups and may need a stronger controller or a biologic therapy.
These ranges aren’t absolute. Your doctor will combine them with your symptoms, lung function, and history. A high FeNO in someone with no symptoms might not need treatment change. A low FeNO in someone with frequent attacks might need other tests.
Real Patient Experiences
Patients who’ve had FeNO testing often say it changed their care.
One mother on Asthma + Lung UK’s forum said: “My 8-year-old had wheezing for years. Spirometry was normal. FeNO was 38 ppb. The allergist said, ‘This is asthma.’ We started a steroid inhaler-and no more missed school.”
Another user on Reddit wrote: “I’d been on three different inhalers for two years. Nothing worked. FeNO showed I was still inflamed. My doctor switched me to a biologic. Within three months, I could run without stopping.”
But not everyone has good access. About 41% of community clinics in the U.S. don’t offer FeNO testing. Insurance coverage is inconsistent-only 58% of commercial plans cover it without prior authorization. Some patients report being denied multiple times, even with frequent hospital visits.
Still, in places where it’s available, adoption is high. In the UK, 85% of asthma clinics use FeNO regularly because NICE guidelines require it. In U.S. academic centers, it’s nearly universal. The gap is mostly about resources and reimbursement, not science.
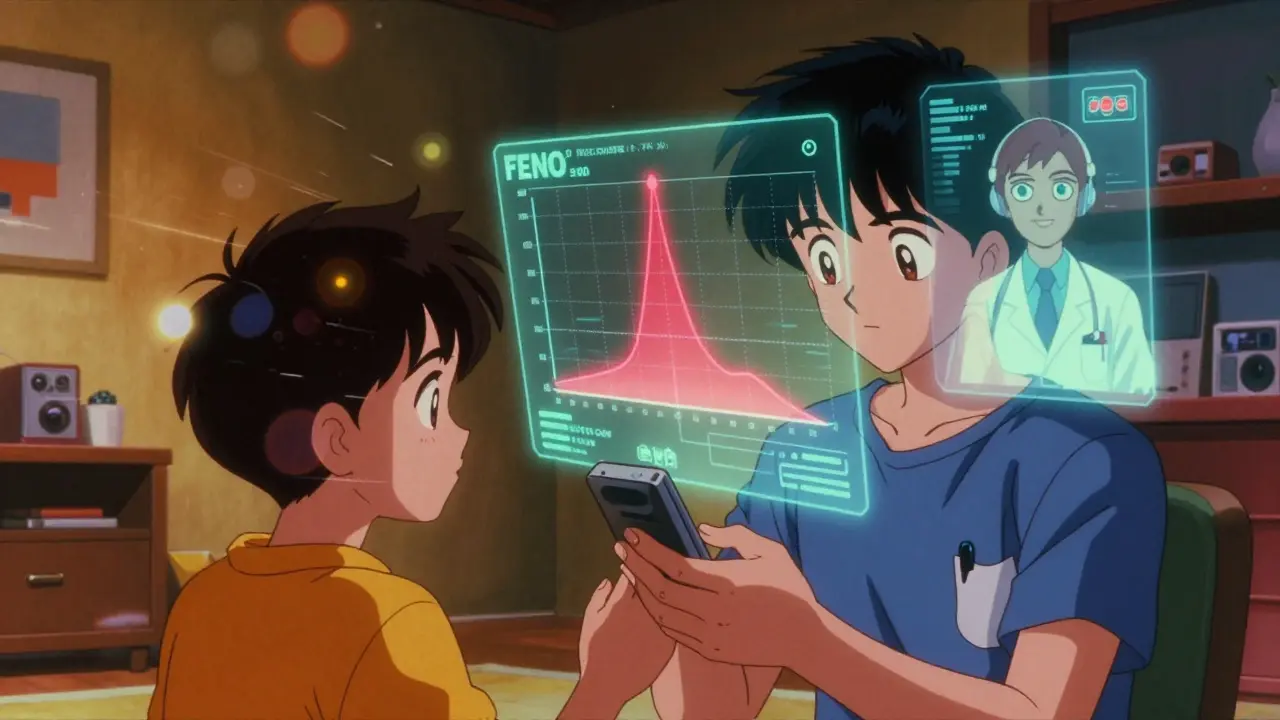
The Future of FeNO: At Home and Online
The biggest shift coming? FeNO testing at home. In early 2023, the FDA cleared the first smartphone-connected FeNO device: Breathometer Asthma. It costs $299 and syncs with an app that tracks your levels over time. You can share the data with your doctor remotely.
This isn’t just convenient-it’s practical. People with severe asthma often need frequent monitoring. Traveling to the clinic every month is costly and time-consuming. Home testing could reduce emergency visits and hospitalizations by letting patients and doctors catch rising inflammation early.
Companies like Circassia and Thermo Fisher are already building platforms that link FeNO devices to electronic health records. Imagine your FeNO level automatically updating your chart, alerting your doctor if it spikes, and suggesting a dose change. That’s not far off.
Who Should Consider FeNO Testing?
You should ask your doctor about FeNO testing if:
- Your asthma symptoms don’t match your treatment
- You’ve been diagnosed with asthma but aren’t responding to standard inhalers
- You’ve had frequent flare-ups or ER visits
- Your doctor suspects you might benefit from a biologic drug
- You’re a child who can’t do spirometry well
It’s not for everyone. If you’re a smoker, have severe COPD, or have non-type 2 asthma, FeNO may not help. But for the majority of people with allergic or eosinophilic asthma, it’s one of the most useful tools in modern care.
Final Thoughts
FeNO testing doesn’t replace your doctor’s judgment. It gives them better data. It turns vague symptoms into measurable numbers. It helps avoid trial-and-error medicine. And it’s one of the few tools in asthma care that directly shows what’s happening inside your airways-without needles, without sputum, without waiting days for lab results.
As biologic therapies become more common-and more expensive-having a simple, reliable way to know who will respond becomes critical. FeNO isn’t magic. But in the right hands, it’s one of the smartest ways to take control of asthma.

Martin Spedding
December 17, 2025 AT 09:51feNo test? sounds like a typo for 'feno' like the italian pasta but ok i guess its some kind of asthma breath thing. my cousin got tested and they said she was 'high' on it so they gave her a new inhaler. now she can't stop coughing. lol.
Naomi Lopez
December 18, 2025 AT 06:52Finally, someone who understands that asthma isn't just 'wheezing and panic.' FeNO is the gold standard for type 2 inflammation-elegant, noninvasive, and biologically grounded. Spirometry is a 1950s relic. If your clinic doesn't offer it, they're practicing prehistoric medicine. And yes, I've read the GINA guidelines. Twice.
Linda Caldwell
December 18, 2025 AT 21:34This is amazing!! I never knew breathing into a tube could change your life. My kid went from missing school every month to acing soccer tryouts. Doctors need to push this harder. No more guesswork. Just breathe and get better. Yes!!
Anna Giakoumakatou
December 19, 2025 AT 20:50Oh wow, another 'miracle diagnostic tool' that costs $3,000 and is only available in Beverly Hills clinics. How quaint. Let me guess-next they’ll tell us to test our tears for serotonin to diagnose depression. The medical-industrial complex never sleeps, does it?
CAROL MUTISO
December 20, 2025 AT 17:55FeNO isn’t just a number-it’s a conversation starter between you and your lungs. I’ve seen patients cry when they finally get proof their suffering isn’t ‘all in their head.’ The tech is simple, the science is solid, and the humanity behind it? That’s the real breakthrough. It’s not about the ppb-it’s about being heard.
Also, if your insurance denies it, fight. Send them the ATS guidelines. Print them. Mail them. Send a carrier pigeon. Do whatever it takes. Your breath matters.
Erik J
December 22, 2025 AT 09:25Is there data on how FeNO correlates with long-term lung function decline? I’m curious if it’s predictive beyond just acute inflammation. Also, how often do false negatives occur in non-type-2 asthma? Just wondering.
BETH VON KAUFFMANN
December 23, 2025 AT 08:19FeNO is essentially a glorified gas chromatograph for the clinically lazy. Eosinophilic inflammation is just one phenotype. You’re ignoring neutrophilic, paucigranulocytic, and obesity-related asthma. The algorithmic overreliance on biomarkers is a dangerous trend. And yes, I’ve published on this in JACI.
Jessica Salgado
December 24, 2025 AT 02:34I’ve been denied FeNO testing three times. My ER visits? Paid for by my parents. My inhaler? Out of pocket. My doctor? Says ‘it’s not medically necessary.’ But when I showed them the 48 ppb result from my private clinic? They changed their tune. Why should access depend on your bank account? This isn’t healthcare. It’s a lottery.
amanda s
December 24, 2025 AT 09:03Why are we letting Europeans and Brits dictate our asthma care? In America, we have real doctors who look you in the eye and listen. Not some $300 gadget that tells you you’re ‘inflamed.’ This is why our kids are growing up thinking they need tech to breathe. We don’t need FeNO. We need discipline. And maybe less gluten.