Pharmacokinetic Interactions: How Drugs Affect Each Other in Your Body
When you take more than one medication, your body doesn’t treat them like separate events—it tries to process them all at once. This is where pharmacokinetic interactions, how drugs change each other’s absorption, distribution, metabolism, or excretion in the body. Also known as drug interactions, it happens long before you feel any effect—right in your liver, kidneys, and gut. These aren’t just theoretical risks. They’re real, measurable, and often silent. One drug might slow down how fast another breaks down, causing toxic levels. Another might block absorption so completely that your pill becomes useless. This isn’t about side effects—it’s about your body’s internal chemistry being rewired by what you swallow.
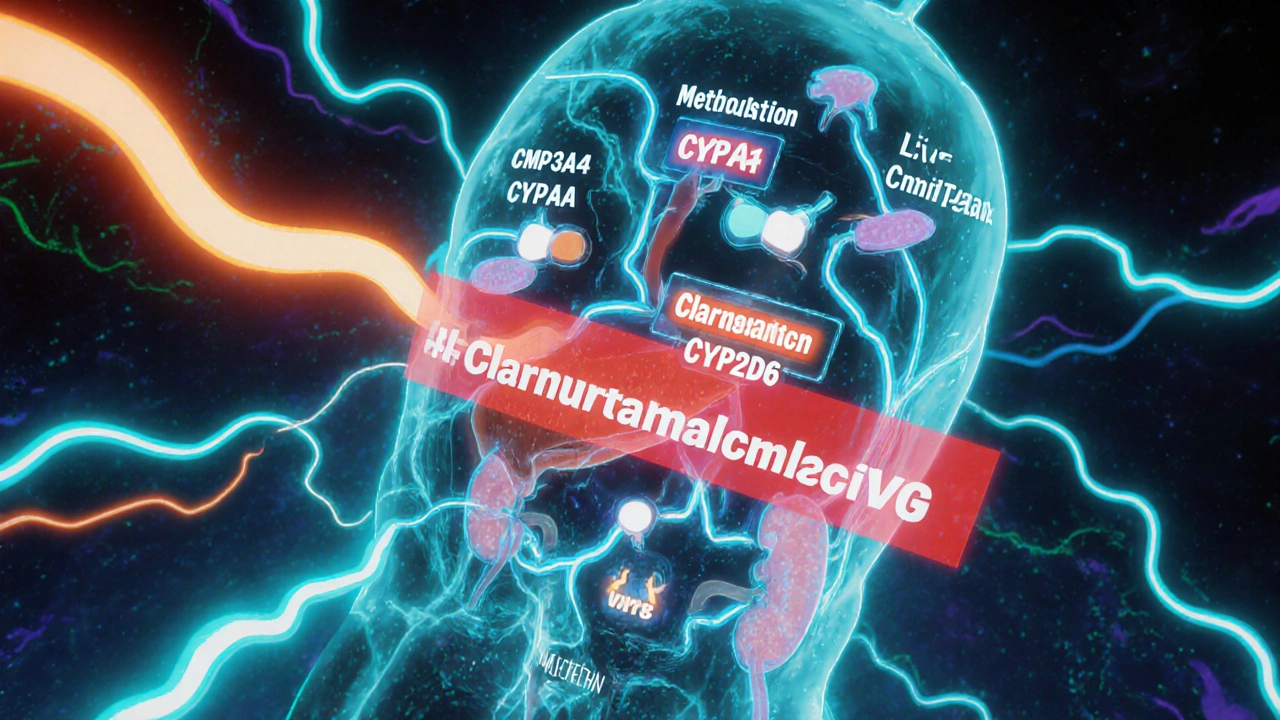
Think of your liver as a busy factory. Drugs like metabolism, the process by which the body breaks down medications using enzymes, especially CYP450. Also known as drug metabolism, it is the main assembly line. If one drug jams the machinery—say, grapefruit juice blocking CYP3A4—other drugs pile up. That’s why mixing PDE5 inhibitors with nitrates can drop your blood pressure to dangerous levels. Or why taking tizanidine with certain antibiotics can turn dizziness into a fall risk. It’s not the drugs themselves being bad—it’s how they interfere with each other’s journey through your system. Absorption matters too. Some antibiotics like norfloxacin won’t work if you take them with calcium-rich foods or antacids. The calcium binds to the drug before it can be absorbed, making your treatment pointless. And excretion? If your kidneys are slowed by another medication, even a normal dose of a drug like tolvaptan can build up and cause dehydration or electrolyte chaos.
These aren’t rare edge cases. They’re daily realities for people managing chronic conditions—diabetes, heart disease, mental health, or chronic pain. That’s why posts here cover everything from how Samsca compares to other diuretics, to why clonidine might help schizophrenia symptoms by altering drug clearance, to why generic drugs sometimes get denied coverage because of how they’re metabolized differently. You’ll find real examples: how isoniazid interacts with rifampin in TB treatment, how SSRIs for OCD need higher doses because of metabolic differences, and why osteoporosis drugs like Actonel need careful timing with calcium supplements. This isn’t guesswork. It’s science you can use. What you’re about to read isn’t just a list of articles—it’s a map to avoid hidden dangers and make sure your meds actually work the way they should.
Pharmacokinetic vs Pharmacodynamic Drug Interactions: What You Need to Know
Understand how pharmacokinetic and pharmacodynamic drug interactions affect your health. Learn the difference, which drugs are risky, and how to stay safe when taking multiple medications.