When you hear the word ranolazine, you might picture a niche drug tucked away on a pharmacy shelf. In reality, it’s become a go‑to option for many patients whose chest pain isn’t fully controlled by the classic drugs. This guide walks through why ranolazine matters, how it fits with other treatments, and what you need to watch out for.
What Is Angina and Why It Needs a Full‑Spectrum Plan
Angina pectoris is the clinical term for the pressure‑like discomfort that pops up when the heart muscle doesn’t get enough oxygen. It’s a symptom of underlying myocardial ischemia, most often caused by atherosclerotic narrowing of the coronary arteries. While lifestyle tweaks-like quitting smoking, eating heart‑healthy meals, and regular aerobic exercise-lay the foundation, pharmacologic therapy is what brings the pain under control day‑to‑day.
Introducing Ranolazine
Ranolazine is an oral anti‑anginal medication that reduces the frequency and severity of chest pain without affecting heart rate or blood pressure. First approved by the FDA in 2006, it works by modulating the late sodium current in cardiac cells, a mechanism distinct from that of beta‑blockers or nitrates.
How Ranolazine Works - The Science Made Simple
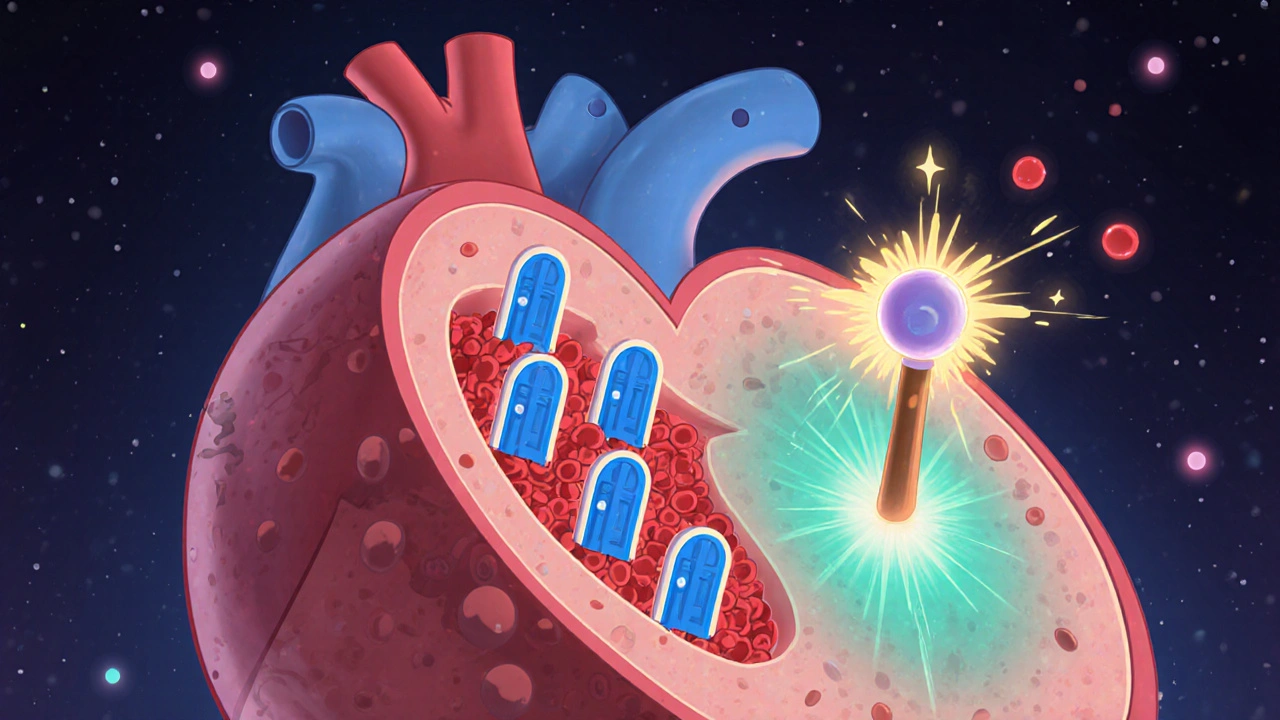
The heart’s electrical activity relies on a delicate balance of sodium and calcium ions. In ischemic tissue, the late sodium current stays open longer than it should, pushing extra sodium inside the cell. This forces the sodium‑calcium exchanger to bring in more calcium, which raises intracellular calcium levels, stiffens the heart muscle, and spikes oxygen demand.
Ranolazine selectively blocks that lingering sodium influx, indirectly lowering calcium overload. The result? The heart uses less oxygen for the same workload, easing the mismatch that triggers angina.
When to Choose Ranolazine - Patient Selection
Guidelines from the American College of Cardiology (ACC) and the European Society of Cardiology (ESC) place ranolazine in the “add‑on” tier. It’s recommended for patients who:
- Remain symptomatic despite optimal doses of a beta‑blocker, calcium‑channel blocker, or nitrate.
- Cannot tolerate higher doses of traditional agents because of low blood pressure or bradycardia.
- Have persistent angina after revascularization (PCI or CABG) but still experience daily episodes.
Because ranolazine does not significantly change heart rate or blood pressure, it’s a safe fallback for the elderly or those with comorbid hypertension.
Comparing Ranolazine with Other Anti‑Anginals
| Drug Class | Primary Mechanism | Typical Dose | Onset of Relief | Major Side Effects |
|---|---|---|---|---|
| Ranolazine | Late sodium current inhibition | 500mg-1000mg BID | 1‑2weeks | Dizziness, constipation, QT‑prolongation |
| Beta‑blocker | β‑adrenergic blockade | Metoprolol 25‑200mg QD | Days | Fatigue, bradycardia, bronchospasm |
| Calcium‑channel blocker | amlodipine, diltiazemAmlodipine 5‑10mg QD | Hours | Peripheral edema, constipation, flushing | |
| Nitrate | Vasodilation via NO | Isosorbide mononitrate 20‑80mg QD | Minutes | Headache, tolerance, hypotension |
Notice how ranolazine’s onset is slower than nitrates but its lack of effect on blood pressure makes it attractive when other drugs cause hypotension.
Practical Dosing and Monitoring
- Start with 500mg twice daily with meals.
- After one week, if angina persists and the patient tolerates the drug, increase to 1000mg twice daily.
- Check baseline ECG for QT interval; repeat after dose escalation.
- Monitor renal function; reduce to 500mg BID if creatinine clearance <30mL/min.
- Educate patients to report palpitations, dizziness, or syncope immediately.
Regular follow‑up every 4-6weeks during titration helps catch QT prolongation early. Most clinicians aim for a target dose that balances symptom relief with tolerability.
Safety Profile - What to Watch For
Ranolazine is generally well‑tolerated, but a few safety signals deserve attention:
- QT prolongation: Avoid using with other QT‑prolonging agents (e.g., certain anti‑arrhythmics, macrolide antibiotics).
- Drug interactions: CYP3A4 and CYP2D6 inhibitors (e.g., ketoconazole, fluoxetine) raise ranolazine levels.
- Renal impairment: Dose reduction is mandatory; severe renal failure may preclude use.
- Gastro‑intestinal symptoms: Constipation and nausea are the most common complaints.
Pregnant or breastfeeding women lack robust safety data, so clinicians usually reserve ranolazine for those who have exhausted other options.

Integrating Ranolazine into a Comprehensive Angina Plan
A modern angina strategy blends three pillars:
- Lifestyle modification - diet, exercise, smoking cessation.
- Revascularization when indicated - PCI or CABG for high‑risk anatomy.
- Pharmacologic therapy - the drug cocktail that keeps symptoms at bay.
Ranolazine slots into the third pillar, usually after beta‑blockers, calcium‑channel blockers, or nitrates have been maximized. Because it doesn’t lower heart rate or blood pressure, it can be layered on top of any of those agents without causing additive hypotension.
Clinical pathways often look like this:
- Start with a beta‑blocker (e.g., metoprolol).
- Add a calcium‑channel blocker if heart rate remains high.
- Introduce a nitrate for breakthrough episodes.
- If angina persists, bring in ranolazine as an add‑on.
This stepwise approach mirrors ACC/AHA guidelines and keeps the medication burden manageable.
Key Takeaways for Clinicians
- Ranolazine reduces ischemic burden by targeting the late sodium current, a unique mechanism among anti‑anginals.
- It’s ideal for patients who can’t tolerate higher doses of beta‑blockers or nitrates because of low blood pressure.
- Start low, go slow, and monitor QT interval; watch for CYP3A4/2D6 interactions.
- Use it as an add‑on after lifestyle changes, revascularization when needed, and first‑line drugs have been optimized.
Frequently Asked Questions
Frequently Asked Questions
Can ranolazine be used alone for angina?
Guidelines advise using ranolazine as an add‑on to at least one other anti‑anginal agent. Its effect is modest when used solo, and most studies evaluated it in combination therapy.
What are the most common side effects?
Mild dizziness, constipation, and nausea occur in about 10‑15% of patients. QT prolongation is rare but clinically important.
Is ranolazine safe for patients with atrial fibrillation?
Because it does not affect heart rate, ranolazine can be used in atrial fibrillation, but clinicians should still monitor for QT changes, especially if patients are on other anti‑arrhythmic drugs.
How does kidney function influence dosing?
If creatinine clearance falls below 30mL/min, the dose should be reduced to 500mg twice daily, and plasma levels may need to be checked.
Can ranolazine be taken with statins?
Yes, no significant interaction has been reported. However, check for CYP3A4 inhibitors that could raise both drug levels.

jana caylor
October 16, 2025 AT 16:13Ranolazine’s unique sodium‑channel action makes it a solid add‑on for stubborn angina, especially when beta‑blockers cause low blood pressure.
Vijendra Malhotra
October 17, 2025 AT 13:20Ranolazine has steadily earned its place in the Indian cardiology toolbox over the past decade.
Many of us have observed patients who cannot tolerate high doses of beta‑blockers due to pre‑existing hypotension.
In such scenarios, the drug’s neutral effect on heart rate and blood pressure becomes a lifesaver.
Our hospitals often start at 500 mg twice daily, mirroring the FDA‑approved regimen, and then titrate up once tolerance is confirmed.
The delayed onset of relief, typically one to two weeks, aligns well with the chronic nature of angina management.
Moreover, the drug’s mechanism-blocking the late sodium current-directly addresses the ionic imbalance that underlies ischemic contracture.
This biochemical nuance explains why patients report smoother exercise tolerance even when their ECG still shows modest ischemic changes.
We have also noted a lower incidence of reflex tachycardia compared with traditional nitrates, which matters for our elderly cohort.
The QT‑prolongation risk, while real, can be mitigated by baseline ECG screening and avoiding concurrent QT‑extending agents.
In practice, we pair ranolazine with low‑dose diltiazem when calcium‑channel blockers are otherwise indicated.
The combination has shown synergistic improvement in angina frequency in several pilot studies from Delhi and Mumbai.
Importantly, ranolazine does not exacerbate renal impairment, provided dose adjustments are made for creatinine clearance below 30 mL/min.
Cost remains a barrier in many public hospitals, yet generic versions are becoming more accessible, reducing the financial strain on patients.
Education on medication adherence is crucial because missing doses can quickly erode the modest benefits.
Our nursing staff has incorporated a simple checklist to verify that patients take the drug with meals, as food helps absorption.
Side‑effects such as constipation and dizziness are generally mild and resolve within a few days of dose stabilization.
When severe side‑effects arise, we do not hesitate to down‑titrate or discontinue, switching to alternative anti‑anginals as needed.
Overall, the integration of ranolazine into a step‑wise angina protocol has markedly improved quality‑of‑life scores across our outpatient clinics.
Nilesh Barandwal
October 18, 2025 AT 10:26Indeed-ranolazine works where others falter; it tames the late sodium surge, calms calcium overload, and restores balance; a quiet hero in the cellular battlefield! The heart, relieved of excess calcium, breathes easier; oxygen demand drops, pain retreats. Patients, once shackled by daily chest tightness, find new rhythm; daily walks become possible again. The drug’s neutrality on heart rate, its sparing of blood pressure, all combine into an elegant solution; it is medicine poetry!
Elise Smit
October 19, 2025 AT 07:33When you add ranolazine to a beta‑blocker regimen, watch for that modest dip in dizziness and keep an eye on the QT interval; a quick ECG check after the first week is all it takes to stay safe and confident.
Sen Đá
October 20, 2025 AT 04:40It is imperative to acknowledge that the pharmacokinetic profile of ranolazine demands rigorous monitoring, particularly in patients with compromised renal function; failure to adjust the dose accordingly may precipitate adverse cardiac events, a circumstance that must be avoided at all costs.
LEE DM
October 21, 2025 AT 01:46From a broader perspective, incorporating ranolazine into community health programs offers a balanced approach-patients gain relief without the blood‑pressure dips that often limit traditional therapy, and clinicians can tailor regimens to diverse populations.
mathokozo mbuzi
October 21, 2025 AT 22:53One observes that the modest cost increase associated with ranolazine is frequently offset by reduced hospital admissions for angina‑related events, a fact that underscores its value in health‑system budgeting.
Penny X
October 22, 2025 AT 20:00Let us not overlook the moral imperative to prescribe ranolazine responsibly, lest we abandon our duty to alleviate suffering.
Michael Ieradi
October 23, 2025 AT 17:06Indeed, responsible prescribing safeguards patient wellbeing.