Heart Failure – What You Need to Know
Did you know that heart failure touches the lives of over 26 million people worldwide? It’s not a one‑time event; it’s a chronic condition where your heart struggles to pump blood efficiently. Understanding it early can change how you feel day to day.
Common Signs and Symptoms
The first clue is usually shortness of breath, especially when you climb stairs or lie flat. You might notice swelling in your ankles, feet, or abdomen—your body’s way of holding onto extra fluid. Fatigue pops up quickly because the heart can’t deliver enough oxygen to muscles.
Weight gain without a clear reason is another red flag; even a couple of pounds over a few days can signal fluid buildup. If you hear a persistent cough, especially at night, it’s often linked to fluid in your lungs. Keep an eye on rapid heartbeat or irregular beats—they’re common when the heart works harder than it should.
Managing Heart Failure at Home
The backbone of everyday management is lifestyle tweaks. Cut sodium dramatically—aim for less than 1,500 mg a day—to keep fluid from pooling. Swap salty snacks for fresh fruits, veggies, or low‑sodium seasonings.
Stay active, but don’t overdo it. A gentle walk three times a week can boost circulation without stressing the heart. Track your daily weight; a sudden rise of more than 2 lb signals you should call your doctor.
Medication adherence is non‑negotiable. Common prescriptions include ACE inhibitors, beta‑blockers, and diuretics—each plays a role in lowering blood pressure, reducing workload, or flushing excess fluid. Set alarms or use a pill organizer to avoid missed doses.
Watch your fluid intake, especially if your doctor limits it. Most patients stay under 1.5–2 liters per day, but the exact number varies. Pair each glass of water with a small snack to keep blood sugar stable and prevent dehydration.
If you smoke, quit now. Smoking narrows arteries and makes the heart work harder. Even occasional vaping can worsen symptoms, so steer clear.
Stress management isn’t just feel‑good fluff; chronic stress releases hormones that raise heart rate and blood pressure. Try simple breathing exercises—inhale for four counts, hold two, exhale six—to calm your nervous system.
Regular check‑ups let doctors fine‑tune your treatment plan. Bring a symptom diary to appointments; noting when breathlessness worsens or swelling appears helps them adjust meds faster.
Lastly, don’t ignore mental health. Living with heart failure can feel overwhelming, and anxiety often amplifies physical symptoms. Talk to a therapist or join a support group—sharing experiences lightens the load.
Heart failure isn’t a life sentence; with the right knowledge, medication, and daily habits, you can keep moving forward and enjoy a better quality of life.
How Blood Pressure Management Helps Treat Left Ventricular Dysfunction
Effective blood pressure management can slow, stop, or even reverse left ventricular dysfunction. Learn how targeted medications and lifestyle changes improve heart function and reduce heart failure risk.
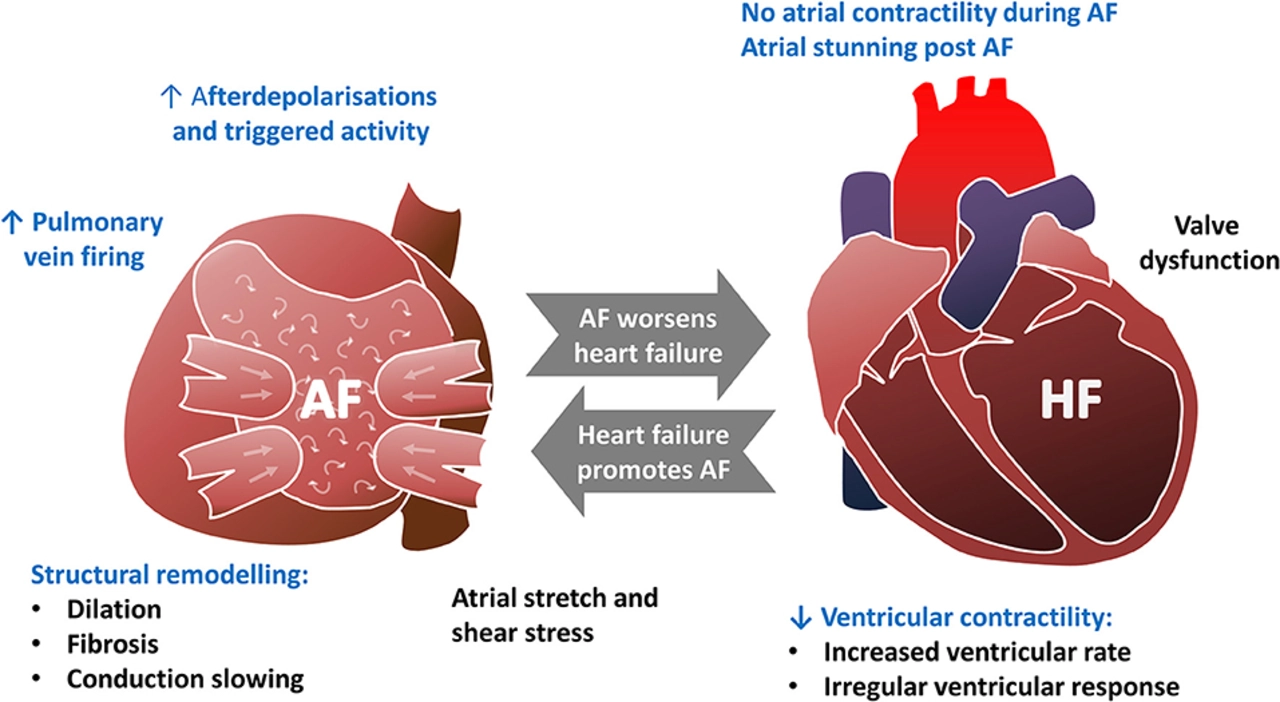
The Connection between Irregular Heartbeat and Heart Failure
I recently came across some interesting information about the connection between irregular heartbeat and heart failure. It turns out that having an irregular heartbeat, also known as arrhythmia, can significantly increase the risk of developing heart failure. This is because arrhythmias disrupt the normal functioning of the heart muscle, making it difficult for the heart to pump blood effectively. Over time, this strain on the heart can lead to heart failure, a condition where the heart can no longer meet the body's demands for oxygen and nutrients. It's a crucial reminder for all of us to pay attention to our heart health and consult a doctor if we experience any irregularities in our heartbeat.