When a pharmacist hands you a prescription, they’re not just giving you pills. They’re handing you a chance to take control of your health. But too often, that chance gets lost in the rush. A 2022 NACDS report found the average counseling session in a community pharmacy lasts just 2.1 minutes. That’s not enough time to explain how a drug works, what side effects to watch for, or why skipping doses can be dangerous. That’s where counseling scripts come in-not as robotic scripts to read, but as safety nets to make sure nothing critical slips through the cracks.
Why Scripts Are Necessary, Not Optional
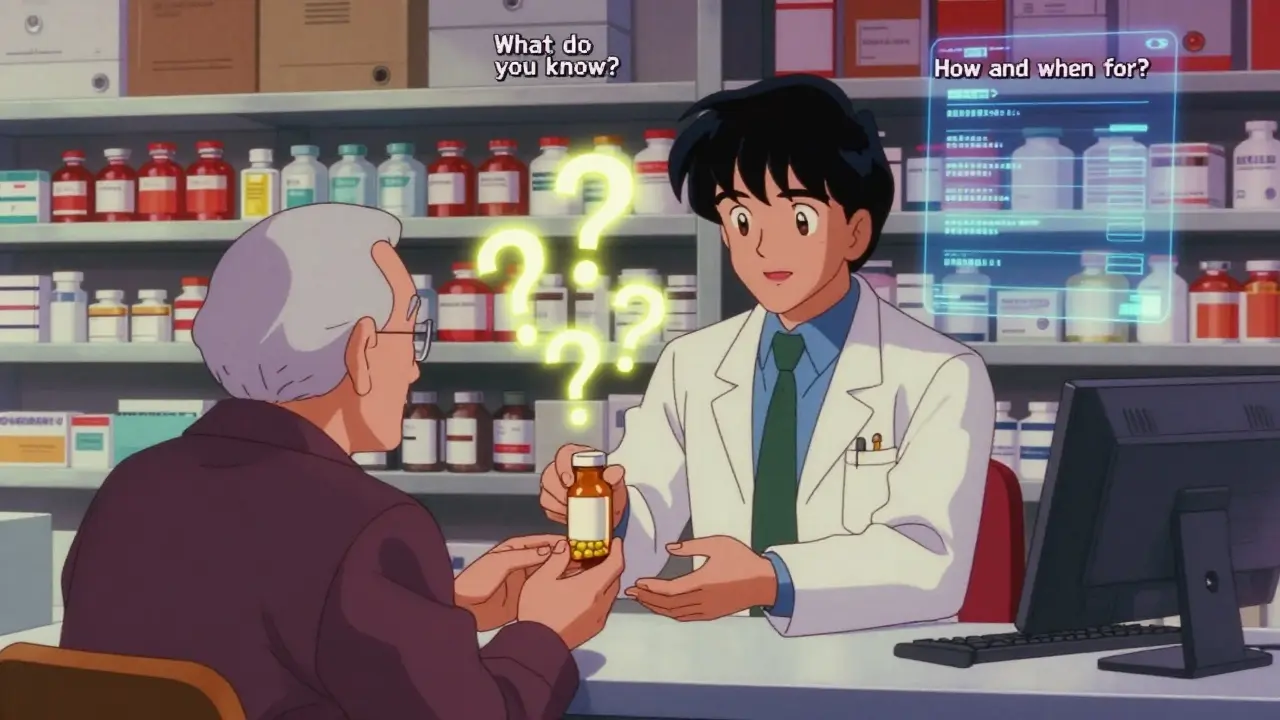
The push for standardized counseling didn’t start with corporate policy. It started with law. The Omnibus Budget Reconciliation Act of 1990 (OBRA '90) made it clear: if a pharmacy wants Medicaid reimbursement, they must counsel patients. Not just offer it. Not just ask if they have questions. Actually counsel them. That single rule changed how pharmacists work. Suddenly, talking to patients wasn’t a nice-to-have-it was a legal requirement. But laws don’t tell you how to talk. That’s where scripts fill the gap. They’re not about reading lines. They’re about making sure the same core information gets delivered every time-whether it’s a new grad on their first day or a veteran pharmacist rushing between 12 patients in an hour. The Indian Health Service model, widely used in training, boils it down to three essential questions:- What do you know about why you’re taking this medicine?
- How and when should you take it?
- What problems should you watch out for?
What’s Actually Required in Every Counseling Session
OBRA '90 didn’t leave room for guesswork. It laid out exactly what must be covered for every new prescription. States have added their own layers since then, but the federal baseline is clear. If you’re counseling a patient, you must cover:- The name and description of the medication
- The dosage form (tablet, liquid, inhaler, etc.)
- The route of administration (by mouth, injection, patch)
- The exact dosage and how often to take it
- How long the therapy should last
- Special directions (take with food? avoid alcohol? store in fridge?)
- Common severe side effects and what to do if they happen
The Difference Between a Script and a Conversation
The biggest mistake pharmacists make is treating scripts like teleprompters. Reading them word-for-word turns a health conversation into a performance. Dr. William Ellis, writing in the Journal of the American Pharmacists Association in 2019, called this “over-scripting.” He saw patients zone out when pharmacists sounded like they were reciting a manual instead of talking to a person. The fix? Use the script as a checklist, not a script. Start with the three core questions. Listen to the answers. Then expand based on what the patient says. If they mention they’re worried about dizziness, don’t just list side effects-ask, “Have you felt dizzy before starting this?” Then tailor the advice. That’s the teach-back method in action: ask the patient to repeat the instructions in their own words. If they say, “I take this when I feel my head spinning,” you know you’ve got a misunderstanding to fix.Special Cases Need Special Scripts
Not all medications are created equal. A script for high blood pressure won’t work for opioids. That’s why specialized scripts exist. For controlled substances like oxycodone or fentanyl patches, the RXCE 2023 training materials require four extra elements:- How to store the medication safely (out of reach of kids or pets)
- How to dispose of unused pills (don’t flush them-use a take-back program)
- Why naloxone should be kept on hand
- Signs of overdose and what to do immediately
How to Train New Pharmacists Without Creating Robots
Pharmacy schools teach counseling using the ASHP guidelines. They’re the gold standard. But new grads often panic when they hit the floor. They’re overwhelmed by volume, confused by state laws, and scared they’ll miss something. That’s why most training programs start with rigid scripts. The University of North Carolina’s 2018 curriculum found that novice pharmacists need 8 to 12 weeks of supervised practice before they stop reading scripts and start having conversations. The trick? Start with the three-question framework. Practice it daily. Then, after two weeks, add one personalization step: “What’s your biggest concern about this medicine?” After four weeks, add another: “Tell me how you usually remember to take your pills.” By week eight, they’re not using scripts anymore-they’re using principles. And that’s the goal. Scripts are training wheels. The moment you can ride without them, you should.Documentation Isn’t Bureaucracy-It’s Protection
Pharmacists hate paperwork. But documentation isn’t just for regulators. It’s for you. If a patient later says, “No one told me this could cause falls,” and you have no record of counseling, you’re exposed. ASHP guidelines say you must document two things:- That counseling was offered and accepted (or refused)
- Your assessment of the patient’s understanding
What Happens When Scripts Fail
Scripts aren’t magic. They break when they’re applied without flexibility. A 2022 Community Pharmacy Foundation survey found that 42% of pharmacists felt “script fatigue”-especially when corporate policies forced them to use rigid, one-size-fits-all scripts that ignored patient literacy, language, or emotional state. One pharmacist in California described spending 22% more time on documentation than the national average because her state required detailed written notes instead of checkboxes. Another in Texas said she avoided counseling high-risk patients altogether because the script didn’t account for dementia. These aren’t failures of the pharmacist-they’re failures of poor design.
The Future: Smarter Scripts, Not More Scripts
The next leap isn’t in more rules. It’s in smarter tools. CVS and Walgreens are testing AI-assisted scripts that listen to patient responses and adjust in real time. If a patient says, “I can’t swallow pills,” the system prompts the pharmacist: “Suggest liquid alternative or crushing options.” If they mention cost concerns, it suggests generic equivalents or savings programs. Early results show a 23% improvement in patient comprehension scores compared to static scripts. That’s not just efficiency-it’s better outcomes. And it’s coming fast. By 2025, CMS will require Medicare Part D plans to document patient comprehension, not just counseling. That means scripts will need to include teach-back verification as a mandatory step.Where to Start Today
If you’re a pharmacist, start with the three-question framework. Practice it until it feels natural. Then add one personalization tactic per week. If you’re a trainer, stop asking students to memorize scripts. Ask them to explain why each question matters. If you’re a pharmacy owner, audit your scripts. Are they helping patients understand-or just helping you avoid liability?Medication non-adherence costs the U.S. system $312 billion a year. That’s not just numbers. It’s people in hospitals because they didn’t know how to take their pills. Good counseling doesn’t just save money. It saves lives. And it starts with a simple, well-used script.
Are pharmacist counseling scripts mandatory by law?
Yes, under OBRA '90, pharmacists must counsel patients on new prescriptions if they’re filling Medicaid prescriptions. Many states have expanded this to all prescriptions. Simply offering to counsel isn’t enough-you must actually provide it and document that it happened.
What are the three essential questions in pharmacist counseling?
The widely used core questions are: (1) What do you know about why you’re taking this medicine? (2) How and when should you take it? (3) What problems should you watch out for? These form the backbone of most training scripts and ensure critical information isn’t missed.
Can pharmacists use scripts for telehealth counseling?
Yes. ASHP and CMS updated guidelines in 2023 to include telehealth counseling standards. Scripts can be adapted for phone or video calls, but pharmacists must still confirm patient understanding-often using the teach-back method. Written materials sent via email or patient portals are also required when in-person interaction isn’t possible.
How do I handle language barriers during counseling?
Use certified medical interpreters-never family members. Many pharmacies partner with services like Language Access Network, which provides translated materials in over 150 languages. Always confirm understanding using the teach-back method, even with interpreters present. Written instructions in the patient’s language are mandatory for compliance.
Do I need a different script for opioids versus blood pressure meds?
Absolutely. Opioid counseling requires additional elements: safe storage, proper disposal, naloxone availability, and overdose signs. RXCE’s 2023 guidelines specify these as mandatory. Blood pressure scripts focus more on long-term adherence, side effects like dizziness, and lifestyle factors. Generic scripts don’t work for high-risk medications.
What’s the teach-back method, and why is it important?
Teach-back means asking the patient to explain the instructions in their own words. For example: “Can you tell me how you’ll take this pill?” If they say, “I take it when I feel dizzy,” they’ve misunderstood. This method catches errors before they become problems and is now required in Medicare Part D plans starting in 2025.
How much time should I spend on counseling?
There’s no fixed time, but OBRA '90 doesn’t specify it. The goal is completeness, not speed. The average is 2.1 minutes, but effective counseling often takes 3-5 minutes. Use scripts to streamline, not rush. If you’re cutting it shorter, you’re risking patient safety.
What’s the best way to document counseling?
Use your pharmacy system’s checkboxes for “counseling offered” and “counseling accepted.” Then add a brief note: “Patient repeated dosage correctly. Asked about food interaction-clarified no issue.” This satisfies legal requirements and protects you if questions arise later.
Next Steps for Pharmacists
Start small. Pick one script-maybe the three-question framework-and use it for every new prescription this week. After seven days, add the teach-back method. Then, review your documentation. Are you just checking boxes, or are you capturing real understanding? If you’re a manager, audit your team’s counseling logs. Are they consistent? Are they human? If not, retrain-not with more rules, but with more practice.The goal isn’t to turn pharmacists into robots. It’s to make sure no patient walks away confused. Because in the end, it’s not about the script. It’s about the person holding the pill bottle-and whether they know what to do with it.
Fabian Riewe
December 29, 2025 AT 17:12Man, I’ve seen pharmacists rush through counseling like they’re on a timer at a fast-food drive-thru. But this? This is the real deal. The three-question framework is low-key genius-simple, human, and actually works. I’ve watched my grandma understand her blood pressure meds after a 90-second chat using this. No jargon, no panic. Just clarity.
And teach-back? That’s the secret sauce. Not ‘do you understand?’ but ‘tell me how you’ll take this.’ Huge difference.
Lisa Dore
December 31, 2025 AT 00:17This is why I love pharmacy. It’s not just dispensing-it’s caring. I’ve trained new techs using the three-question method, and within weeks, they’re not reading scripts-they’re having conversations. One kid even started asking patients, ‘What’s your biggest worry about this pill?’-and that’s when the magic happens.
Scripts aren’t robots. They’re scaffolding. Take ‘em down when you’re ready, but don’t skip the build.
Sharleen Luciano
December 31, 2025 AT 21:14Let’s be real-most pharmacists can’t even spell ‘compliance’ correctly, let alone counsel properly. These ‘scripts’ are just corporate bandaids slapped on a broken system. OBRA ‘90 was a noble idea, but now it’s just another checkbox in an EHR that no one reads.
And don’t get me started on ‘teach-back.’ If your patient can’t articulate the dosage, maybe they shouldn’t be taking it. Stop pretending a script fixes poor health literacy. It doesn’t. It just hides the problem.
Jim Rice
January 2, 2026 AT 15:40Wait-so you’re telling me we’re giving pharmacists a script to talk to patients… but they’re not allowed to read it? That’s not a script. That’s a paradox. Why not just train them to talk? Why force them into this weird half-measure? It’s like giving a chef a recipe but telling them not to follow it.
And why are we even talking about ‘scripts’? This isn’t theater. It’s medicine. If you can’t explain a pill in 2 minutes, you’re not qualified to hand it out. End of story.
Henriette Barrows
January 2, 2026 AT 20:06I work in a rural clinic, and I’ve seen patients cry because they didn’t know their med was supposed to be taken on an empty stomach. They thought ‘once daily’ meant ‘whenever I remember.’
This isn’t about legal compliance. It’s about dignity. Every person deserves to know what they’re putting in their body. The three-question method? It’s not perfect-but it’s the first thing that actually makes people feel heard.
Also, naloxone scripts? Life-saving. Not just for the patient. For their whole family.
Aliza Efraimov
January 3, 2026 AT 01:30AI-assisted scripts are the future-and honestly, long overdue. I’ve used a prototype system at my clinic that adapts based on patient tone. If someone says ‘I hate pills,’ it auto-suggests liquid options or patches. If they mention cost, it pulls up coupons in real time.
One patient said, ‘I didn’t know I could get this for $4.’ She almost hugged the pharmacist. That’s not tech. That’s care with a UI.
And yes-2025 is coming. CMS is going to demand proof of understanding. No more ‘counseling provided’ checkboxes. We’re either ready or we’re falling behind.
Nisha Marwaha
January 4, 2026 AT 11:36From an Indian healthcare systems perspective, the OBRA ‘90 framework is remarkably aligned with the National Health Mission’s patient education protocols. The three-question model mirrors our ‘Know-Ask-Repeat’ triad used in ASHA worker training.
However, the critical gap in Western models is the absence of cultural context in script design. For example, in rural India, ‘take with food’ often means ‘take with rice,’ not ‘take with a meal.’ Scripts must localize idioms, not just translate them.
Also, the reliance on EHR checkboxes ignores the fact that 60% of our patients are illiterate. Teach-back must be visual-drawings, pictograms, gestures. Text-based compliance is a myth.
Paige Shipe
January 5, 2026 AT 22:56I work in a pharmacy and I have to say I think this whole script thing is a joke. We have 12 patients an hour and they expect us to be therapists too? No thanks. I just hand them the bottle and say ‘take as directed.’ If they don’t understand, that’s not my problem.
Also, who even reads these guidelines? No one. It’s all just paperwork to make lawyers happy. I’ve been doing this for 15 years and I’ve never been sued. So why change?
Tamar Dunlop
January 6, 2026 AT 07:08While the pragmatic utility of standardized counseling frameworks is indisputable, one must not overlook the epistemological limitations inherent in reducing patient education to algorithmic protocols. The ontological integrity of the therapeutic encounter is compromised when the human element is subordinated to procedural compliance.
Furthermore, the imposition of linguistic norms-particularly in multilingual contexts-risks exacerbating epistemic injustice. A script, however well-intentioned, cannot account for the phenomenological experience of illness, nor the cultural semiotics of medication adherence.
One must therefore advocate for a hermeneutic approach to counseling, wherein the script serves not as a directive, but as a heuristic scaffold for emergent dialogue.
David Chase
January 8, 2026 AT 06:39OH MY GOD. Another article about ‘scripts’?!?!?!? We’re in 2025, not 1990! Why are we still talking about OBRA like it’s the Ten Commandments?!?!!?
Look-I’ve worked in 7 states. None of this matters if the patient is on 12 meds, can’t read, and doesn’t have a phone. You think a script fixes THAT?!? You’re delusional.
And AI? Please. If my grandma can’t use Alexa, she’s not gonna trust some robot telling her how to take her blood pressure pills. Stop trying to tech your way out of a systemic failure.
Also-naloxone? That’s a cop-out. We should be fixing the opioid crisis, not handing out free antidotes like candy. 😡💊
Russell Thomas
January 9, 2026 AT 07:54So let me get this straight-you want pharmacists to be part therapist, part lawyer, part AI assistant… and still get paid minimum wage? 😂
Yeah, I’m sure the guy working 12-hour shifts with no breaks is just dying to ask, ‘What’s your biggest concern?’ while 17 people are yelling at him to hurry up.
This isn’t counseling. It’s performance art. And the script? It’s the cue card for a play no one wants to watch.
Joe Kwon
January 10, 2026 AT 06:04I’ve used the three-question method for 3 years now. Started as a new grad, terrified I’d mess up. Now? I barely think about the script. It’s just how I talk.
And the teach-back? Game-changer. One guy said he took his diabetes med ‘when my sugar feels low’-so I asked him to describe what that feels like. Turns out he thought ‘low’ meant ‘tired.’ He’d been taking it at night.
That’s not a failure of the script. That’s proof it works. It’s not about perfection. It’s about catching the stuff that slips through.
Also-shoutout to the pharmacist who taught me this. I owe her everything.
Nicole K.
January 11, 2026 AT 01:41This is disgusting. You’re telling pharmacists to talk to patients like they’re children? What about personal responsibility? If someone can’t follow simple instructions, maybe they shouldn’t be on meds. This is enabling. We’re turning healthcare into a babysitting service.
And why do we keep giving out free stuff? Naloxone? Why not just let people face the consequences of their choices? This is socialism in a pill bottle.
Fabian Riewe
January 12, 2026 AT 08:26Just read Nisha’s comment about India. That’s the real insight. A script that works in Ohio won’t work in Delhi because ‘take with food’ means something totally different.
And Amy’s long-winded post? Yeah, she’s right. But she’s also missing the point. It’s not about the language-it’s about the listening.
Maybe the real script isn’t in the EHR. Maybe it’s in the silence after you ask, ‘What’s your biggest worry?’
That’s when the patient tells you the truth.