Every year, millions of Americans stop taking their medications-not because they feel better, but because they don’t understand what they’re taking. And a big part of that confusion? Generic medications.
You’ve probably seen it: your doctor prescribes a drug, you pick it up at the pharmacy, and the pill looks nothing like the one you got last month. Different color. Different shape. Different markings. You might even see a new name on the bottle. If you’re like most people, your first thought isn’t, ‘This is the same medicine.’ It’s, ‘Did they give me the wrong thing?’
That’s not paranoia. It’s a gap in health literacy-and it’s costing lives and money.
What Exactly Is Health Literacy?
Health literacy isn’t just about reading. It’s about understanding what you read, asking the right questions, and making decisions based on what you learn. The CDC says only 12% of U.S. adults have proficient health literacy. That means nearly nine out of ten people struggle with basic health information-like prescription labels, dosage instructions, or whether a generic pill is safe to take.
When it comes to medications, health literacy includes:
- Reading and understanding pill labels
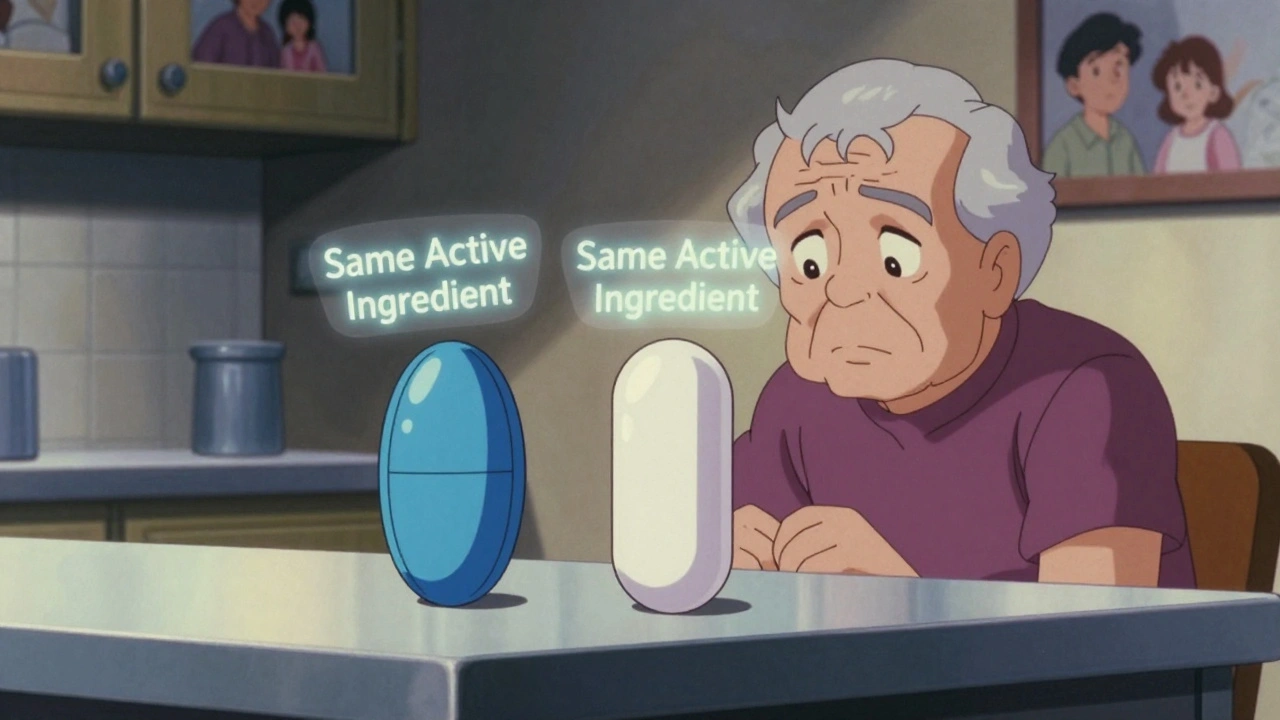
- Knowing what ‘active ingredient’ means
- Calculating doses correctly
- Asking your pharmacist why your medicine looks different
- Using apps or websites to check if a generic is equivalent
But here’s the catch: most people never learn these skills. Schools don’t teach them. Doctors assume you know. Pharmacists are rushed. And when you’re sick, stressed, or elderly, your brain isn’t in ‘learning mode’-it’s in ‘survival mode.’
Why Generics Are So Confusing
Generic drugs are not cheaper because they’re worse. They’re cheaper because they don’t need to pay for advertising, fancy packaging, or years of clinical trials. The FDA requires them to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also be absorbed into the body at the same rate and extent-within a 90% confidence interval of 80-125%. That’s called bioequivalence.
But here’s what most patients don’t know:
- Generics can have different fillers, dyes, or coatings (inactive ingredients)
- These differences can cause side effects in rare cases-like stomach upset or allergic reactions
- They are NOT the same pill visually, even if they work the same way
- They are just as safe and effective as brand-name drugs
Yet, 68% of patients still believe generics are less effective. Why? Because they’ve never been told otherwise.
One study found that 47% of people with low health literacy couldn’t tell that generics contain the same active ingredient as brand-name drugs. That’s not ignorance. That’s a failure of communication.
The Real Cost of Not Understanding
When patients stop taking their meds because they think the generic doesn’t work, the consequences are real:
- They’re 32% more likely to be hospitalized due to medication errors
- They’re 2.5 times more likely to make dangerous mistakes-like taking double doses or skipping refills
- Medication non-adherence costs the U.S. healthcare system between $106 billion and $238 billion every year
And it’s not just about money. For someone managing high blood pressure, diabetes, or depression, stopping their meds can mean a stroke, a coma, or a suicide attempt.
One patient on Reddit said she stopped her blood pressure medication because the generic looked different. Her pharmacist had to explain it was the same drug. She was lucky she found out before her blood pressure spiked.
Another person thought switching to a generic antidepressant meant she was on a new drug. She almost overdosed because she didn’t realize she was already taking the same chemical.
These aren’t rare stories. They’re the norm.
Who’s Most at Risk?
This isn’t a problem that affects everyone equally. Certain groups face much higher risks:
- Older adults-especially those taking five or more medications
- People with limited English proficiency
- Immigrants unfamiliar with U.S. pharmacy systems
- Those with lower income or education levels
- People with cognitive impairments or mental health conditions
Research shows immigrants and non-English speakers are 3.2 times more likely to misunderstand generic medication instructions. Why? Labels are written in complex medical language. Instructions are printed in tiny font. Pharmacists don’t always have interpreters on hand. And many patients are too embarrassed to say, ‘I don’t understand.’
It’s not their fault. It’s the system’s failure.
What Works: Real Solutions That Help
There are proven ways to fix this. But they require effort-from doctors, pharmacists, pharmacies, and even tech companies.
1. The Teach-Back Method
This is simple, powerful, and underused. Instead of saying, ‘Do you understand?’-which most people say yes to just to end the conversation-healthcare providers ask: ‘Can you tell me in your own words how you’ll take this medicine?’
Studies show this reduces misunderstandings by 42%. When patients explain back what they heard, providers catch gaps immediately. One patient said, ‘My pharmacist asked me to show her how I’d take my pills. I said I’d take two in the morning. She noticed I was mixing up the generic and brand names. We fixed it right there.’
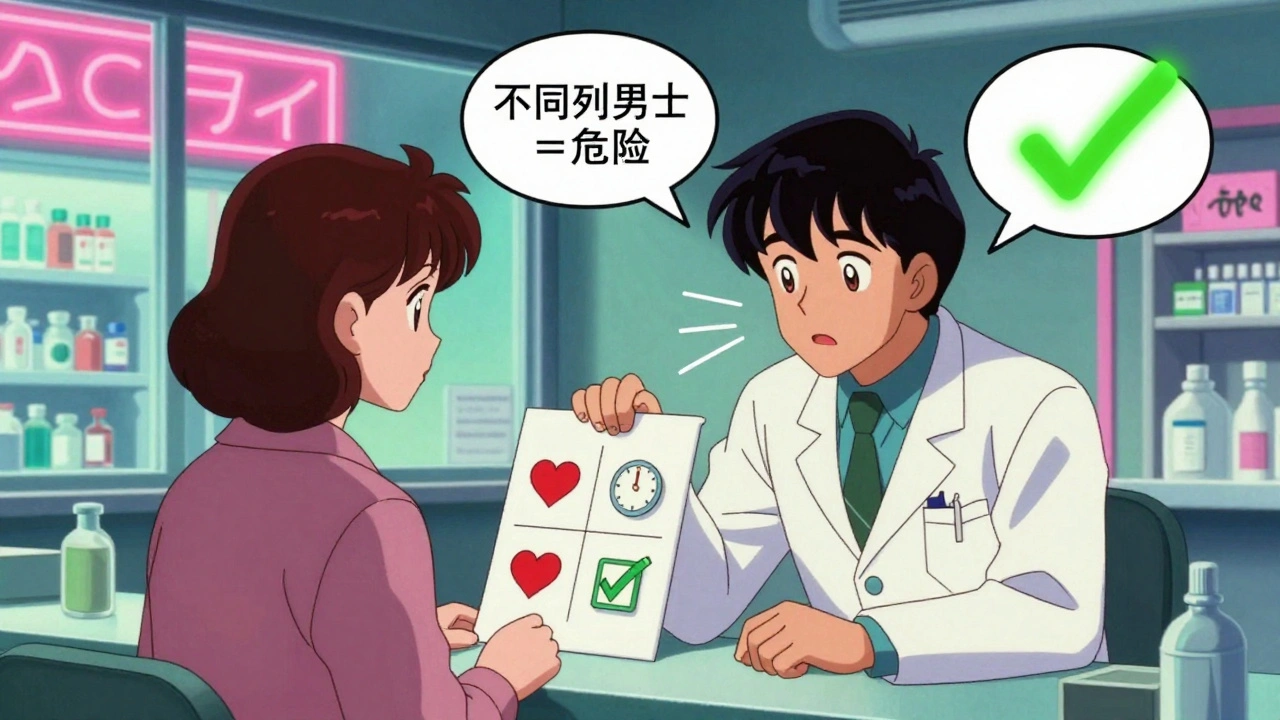
2. Visual Aids and Pill Comparisons
Picture this: a handout with two photos-one of the brand-name pill, one of the generic. Side by side. With labels saying: ‘Same active ingredient. Different shape. Same effect.’
A 2022 study found patients using these visual tools had 35% better recognition of generics than those who only got verbal instructions.
3. Plain Language Labels
Forget ‘Take one tablet by mouth daily.’ Try: ‘Take one pill every day, at the same time.’
Organizations that switched to plain language saw a 29% drop in medication errors and a 22% rise in adherence. Simple words. Clear instructions. No jargon.
4. Digital Tools That Actually Help
Apps that let you scan a pill and see its name, use, and whether it’s generic or brand? They exist. One tool showed patients photos of their pills and asked, ‘Is this the same as your last one?’ Those who used it were far less likely to quit their meds.
But here’s the catch: these tools only work if people know to use them-and if they’re easy to access.
What Pharmacies and Doctors Are (Not) Doing
Pharmacists spend an average of 4.2 minutes explaining a generic substitution. But if the patient has low health literacy? That jumps to 9.7 minutes. That’s not a failure of the pharmacist. It’s a failure of the system. Most pharmacies don’t have the time, training, or resources to do this well.
Doctors? They rarely talk about generics unless the patient asks. And most patients don’t ask because they assume the doctor already explained it.
Only 38% of healthcare organizations have any formal program to teach patients about generics. That’s not enough.
The Bigger Picture: Why This Matters Beyond the Pill
Generics make up 90% of all prescriptions filled in the U.S.-but only 23% of total drug spending. That’s how we save billions. But if patients don’t trust them, they’ll pay more for brand-name drugs-even when their insurance won’t cover them.
That’s not just a waste of money. It’s a waste of health.
When people can’t afford their meds, they skip doses. When they think the generic doesn’t work, they stop. When they’re afraid to switch, they stay on expensive drugs they don’t need.
It’s a cycle: low health literacy → mistrust of generics → non-adherence → hospitalizations → higher costs → less funding for education → worse literacy.
Breaking that cycle isn’t about more pamphlets. It’s about changing how we talk about medicine.
What You Can Do Right Now
If you or someone you care about takes medication, here’s what to do:
- When you get a new prescription, ask: ‘Is this brand-name or generic?’
- If it’s generic, ask: ‘What’s the active ingredient?’ Write it down.
- Compare the pill you got this time to the last one. Take a photo if you need to.
- Ask your pharmacist: ‘Are these the same medicine?’ Don’t be shy.
- Use the Teach-Back method: ‘So, I take one pill every morning, even if I feel fine?’
- Check your pharmacy’s app or website-they often have pill images and explanations.
If you’re a caregiver, family member, or friend-help them ask these questions. Don’t assume they understand. Don’t wait for them to say something’s wrong.
The Future Is Plain Language
The FDA launched its Generics Awareness Campaign in 2023. The CDC added ‘improving understanding of medication alternatives’ to its 2023 Health Literacy Action Plan. Medicare Part D now requires health literacy assessments for plans starting in 2024.
These are steps forward. But real change happens at the counter, in the clinic, in the home.
Health literacy isn’t a patient problem. It’s a system problem. And closing the knowledge gap around generics isn’t just about saving money. It’s about saving lives.
Because a pill that works shouldn’t be a mystery. It should be clear. Simple. Understandable. For everyone.
Tommy Watson
December 14, 2025 AT 01:33bro i took my blood pressure med and it looked like a fucking rainbow gummy bear. i thought i got ripped off or something. turned out it was the generic. now i just take it with a shot of whiskey and pretend it’s a candy.
Donna Hammond
December 15, 2025 AT 00:22This is one of the most important posts I’ve read all year. Health literacy isn’t optional-it’s life-or-death. I’m a pharmacist, and I’ve seen too many patients stop meds because they didn’t recognize the pill. We need plain-language labels, visual guides at the counter, and mandatory teach-backs. No more assumptions. No more ‘do you understand?’-ask ‘how will you take this?’ Every single time.
It’s not about dumbing things down. It’s about speaking clearly. And if we do that, adherence jumps, hospitalizations drop, and lives get saved.
Richard Ayres
December 15, 2025 AT 19:03It’s striking how deeply systemic this issue is. The burden of understanding complex medical information is placed entirely on the patient, often during moments of vulnerability. The fact that 88% of Americans struggle with basic health literacy suggests a cultural failure-not an individual one. We’ve outsourced responsibility for health education to overworked clinicians while ignoring the need for structural change.
Perhaps the most promising solution is not just better labeling, but integrating health literacy training into public education from middle school onward. Imagine if kids learned how to read a prescription label as part of biology class. That’s the kind of shift that could change generations.
Karen Mccullouch
December 17, 2025 AT 09:40Jennifer Taylor
December 18, 2025 AT 00:32Okay but have you ever tried to explain to your 78-year-old grandma that the blue pill she’s been taking for 10 years is now a white oval with ‘A12’ on it and it’s ‘the same thing’? She thinks she’s being poisoned. She cries. She hides the pills. She Googles ‘is this a death pill?’ and then calls 911. I’ve lived this. I’ve been the one holding her hand while she hyperventilates because the pharmacy switched her blood thinner.
And now the system wants to save money by making us all pharmacists? No. We need trained navigators. We need someone to sit with people. Not a pamphlet. Not an app. A person. A real, warm, patient human who says, ‘It’s okay. I’ve got you.’
I’m not mad. I’m just… tired.
sharon soila
December 19, 2025 AT 09:01Understanding your medicine is not a privilege. It’s a right. And right now, the system is failing millions of people who are too scared, too tired, or too overwhelmed to ask questions.
You don’t need a degree to know that a pill should make you feel better-not confused, afraid, or guilty. We can fix this. Not with more jargon. Not with more apps. But with kindness. With patience. With the courage to say, ‘Let me explain this again.’
Every time you ask, ‘What’s this pill?’ you’re not being difficult. You’re being brave. And you deserve an answer that doesn’t make you feel stupid.
Rawlson King
December 20, 2025 AT 08:25Let’s be blunt: this isn’t a literacy issue. It’s a cultural one. Americans expect everything to be handed to them on a silver platter-medications, instructions, emotional support-and then act surprised when they’re confused. If you can’t read a label, maybe you shouldn’t be managing your own prescriptions. Family members, caregivers, or pharmacists should step in. This isn’t rocket science. It’s basic responsibility.
Stop blaming the system. Start taking ownership. Or get someone who can.
Keasha Trawick
December 22, 2025 AT 05:19Let’s talk bioequivalence. The FDA’s 80–125% range? That’s a 45% swing in absorption. For a drug with a narrow therapeutic index-like warfarin, levothyroxine, or phenytoin-that’s not just a ‘maybe.’ That’s a clinical minefield.
And don’t get me started on the fillers. Croscarmellose sodium, magnesium stearate, titanium dioxide-these aren’t inert. Some people have silent reactions. I’ve seen patients develop rashes, GI distress, even migraines after switching generics. No one tracks it. No one connects the dots. The system treats pills like interchangeable Lego blocks.
It’s not that generics are unsafe-it’s that we’ve normalized a dangerous assumption. We act like biology is a spreadsheet. It’s not. And until we stop pretending it is, people are going to get hurt.
Webster Bull
December 22, 2025 AT 16:48my grandma didn’t know her generic was the same as her brand. she thought she was getting weaker meds. she stopped taking it for 3 weeks. her heart went nuts. we had to rush her to the er. just ask. take a pic. say it out loud. it’s not hard.
Bruno Janssen
December 24, 2025 AT 09:24I used to be fine with generics. Until I switched and started having panic attacks. No one told me the dye changed. I thought I was going crazy. Turns out, it was the food coloring. Now I pay extra for brand names. Worth it. No one cares how I feel. Just save money.
Deborah Andrich
December 25, 2025 AT 14:42Cole Newman
December 26, 2025 AT 01:38you think this is bad? try being a diabetic and switching generics and suddenly your sugar goes nuts. no one tells you the fillers affect absorption. the FDA says it’s fine but my glucose monitor says otherwise. i’m not dumb. i’m just tired of being a guinea pig for corporate savings.
Casey Mellish
December 27, 2025 AT 11:38As an Aussie, I’m shocked Americans still struggle with this. Here, pharmacists are required to give a 5-minute verbal briefing on every new script-no exceptions. We even have pill charts with photos on the wall behind the counter. It’s standard. It’s simple. It works. Why is this so hard in the U.S.? Because you’ve turned healthcare into a profit game, not a human one.
It’s not about money. It’s about respect.